Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals

You are here
- Volume 13, Issue 8
- Clinical course of a 66-year-old man with an acute ischaemic stroke in the setting of a COVID-19 infection
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-7441-6952 Saajan Basi 1 , 2 ,
- Mohammad Hamdan 1 and
- Shuja Punekar 1
- 1 Department of Stroke and Acute Medicine , King's Mill Hospital , Sutton-in-Ashfield , UK
- 2 Department of Acute Medicine , University Hospitals of Derby and Burton , Derby , UK
- Correspondence to Dr Saajan Basi; saajan.basi{at}nhs.net
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater oxygen requirement, alongside reduced levels of consciousness. A positive COVID-19 throat swab, in addition to bilateral pneumonia on chest X-ray and lymphopaenia in his blood tests, confirmed a diagnosis of COVID-19 pneumonia. A proactive decision was made involving the patients’ family, ward and intensive care healthcare staff, to not escalate care above a ward-based ceiling of care. The patient died 5 days following admission under the palliative care provided by the medical team.
- respiratory medicine
- infectious diseases
- global health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bcr-2020-235920
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is a new strain of coronavirus that is thought to have originated in December 2019 in Wuhan, China. In a matter of months, it has erupted from non-existence to perhaps the greatest challenge to healthcare in modern times, grinding most societies globally to a sudden halt. Consequently, the study and research into SARS-CoV-2 is invaluable. Although coronaviruses are common, SARS-CoV-2 appears to be considerably more contagious. The WHO figures into the 2003 SARS-CoV-1 outbreak, from November 2002 to July 2003, indicate a total of 8439 confirmed cases globally. 1 In comparison, during a period of 4 months from December 2019 to July 2020, the number of global cases of COVID-19 reached 10 357 662, increasing exponentially, illustrating how much more contagious SARS-CoV-2 has been. 2
Previous literature has indicated infections, and influenza-like illness have been associated with an overall increase in the odds of stroke development. 3 There appears to be a growing correlation between COVID-19 positive patients presenting to hospital with ischaemic stroke; however, studies investigating this are in progress, with new data emerging daily. This patient report comments on and further characterises the link between COVID-19 pneumonia and the development of ischaemic stroke. At the time of this patients’ admission, there were 95 positive cases from 604 COVID-19 tests conducted in the local community, with a predicted population of 108 000. 4 Only 4 days later, when this patient died, the figure increased to 172 positive cases (81% increase), illustrating the rapid escalation towards the peak of the pandemic, and widespread transmission within the local community ( figure 1 ). As more cases of ischaemic stroke in COVID-19 pneumonia patients arise, the recognition and understanding of its presentation and aetiology can be deciphered. Considering the virulence of SARS-CoV-2 it is crucial as a global healthcare community, we develop this understanding, in order to intervene and reduce significant morbidity and mortality in stroke patients.
- Download figure
- Open in new tab
- Download powerpoint
A graph showing the number of patients with COVID-19 in the hospital and in the community over time.
Case presentation
A 66-year-old man presented to the hospital with signs of left-sided weakness. The patient had a background of chronic obstructive pulmonary disease (COPD), atrial fibrillation and had one previous ischaemic stroke, producing left-sided haemiparesis, which had completely resolved. He was a non-smoker and lived in a house. The patient was found slumped over on the sofa at home on 1 April 2020, by a relative at approximately 01:00, having been seen to have no acute medical illness at 22:00. The patients’ relative initially described disorientation and agitation with weakness noted in the left upper limb and dysarthria. At the time of presentation, neither the patient nor his relative identified any history of fever, cough, shortness of breath, loss of taste, smell or any other symptoms; however, the patient did have a prior admission 9 days earlier with shortness of breath.
The vague nature of symptoms, entwined with considerable concern over approaching the hospital, due to the risk of contracting COVID-19, created a delay in the patients’ attendance to the accident and emergency department. His primary survey conducted at 09:20 on 1 April 2020 demonstrated a patent airway, with spontaneous breathing and good perfusion. His Glasgow Coma Scale (GCS) score was 15 (a score of 15 is the highest level of consciousness), his blood glucose was 7.2, and he did not exhibit any signs of trauma. His abbreviated mental test score was 7 out of 10, indicating a degree of altered cognition. An ECG demonstrated atrial fibrillation with a normal heart rate. His admission weight measured 107 kg. At 09:57 the patient required 2 L of nasal cannula oxygen to maintain his oxygen saturations between 88% and 92%. He started to develop agitation associated with an increased respiratory rate at 36 breaths per minute. On auscultation of his chest, he demonstrated widespread coarse crepitation and bilateral wheeze. Throughout he was haemodynamically stable, with a systolic blood pressure between 143 mm Hg and 144 mm Hg and heart rate between 86 beats/min and 95 beats/min. From a neurological standpoint, he had a mild left facial droop, 2/5 power in both lower limbs, 2/5 power in his left upper limb and 5/5 power in his right upper limb. Tone in his left upper limb had increased. This patient was suspected of having COVID-19 pneumonia alongside an ischaemic stroke.
Investigations
A CT of his brain conducted at 11:38 on 1 April 2020 ( figure 2 ) illustrated an ill-defined hypodensity in the right frontal lobe medially, with sulcal effacement and loss of grey-white matter. This was highly likely to represent acute anterior cerebral artery territory infarction. Furthermore an oval low-density area in the right cerebellar hemisphere, that was also suspicious of an acute infarction. These vascular territories did not entirely correlate with his clinical picture, as limb weakness is not as prominent in anterior cerebral artery territory ischaemia. Therefore this left-sided weakness may have been an amalgamation of residual weakness from his previous stroke, in addition to his acute cerebral infarction. An erect AP chest X-ray with portable equipment ( figure 3 ) conducted on the same day demonstrated patchy peripheral consolidation bilaterally, with no evidence of significant pleural effusion. The pattern of lung involvement raised suspicion of COVID-19 infection, which at this stage was thought to have provoked the acute cerebral infarct. Clinically significant blood results from 1 April 2020 demonstrated a raised C-reactive protein (CRP) at 215 mg/L (normal 0–5 mg/L) and lymphopaenia at 0.5×10 9 (normal 1×10 9 to 3×10 9 ). Other routine blood results are provided in table 1 .
CT imaging of this patients’ brain demonstrating a wedge-shaped infarction of the anterior cerebral artery territory.
Chest X-ray demonstrating the bilateral COVID-19 pneumonia of this patient on admission.
- View inline
Clinical biochemistry and haematology blood results of the patient
Interestingly the patient, in this case, was clinically assessed in the accident and emergency department on 23 March 2020, 9 days prior to admission, with symptoms of shortness of breath. His blood results from this day showed a CRP of 22 mg/L and a greater lymphopaenia at 0.3×10 9 . He had a chest X-ray ( figure 4 ), which indicated mild radiopacification in the left mid zone. He was initially treated with intravenous co-amoxiclav and ciprofloxacin. The following day he had minimal symptoms (CURB 65 score 1 for being over 65 years). Given improving blood results (declining CRP), he was discharged home with a course of oral amoxicillin and clarithromycin. As national governmental restrictions due to COVID-19 had not been formally announced until 23 March 2020, and inconsistencies regarding personal protective equipment training and usage existed during the earlier stages of this rapidly evolving pandemic, it is possible that this patient contracted COVID-19 within the local community, or during his prior hospital admission. It could be argued that the patient had early COVID-19 signs and symptoms, having presented with shortness of breath, lymphopaenia, and having had subtle infective chest X-ray changes. The patient explained he developed a stagnant productive cough, which began 5 days prior to his attendance to hospital on 23 March 2020. He responded to antibiotics, making a full recovery following 7 days of treatment. This information does not assimilate with the typical features of a COVID-19 infection. A diagnosis of community-acquired pneumonia or infective exacerbation of COPD seem more likely. However, given the high incidence of COVID-19 infections during this patients’ illness, an exposure and early COVID-19 illness, prior to the 23 March 2020, cannot be completely ruled out.
Chest X-ray conducted on prior admission illustrating mild radiopacification in the left mid zone.
On the current admission, this patient was managed with nasal cannula oxygen at 2 L. By the end of the day, this had progressed to a venturi mask, requiring 8 L of oxygen to maintain oxygen saturation. He had also become increasingly drowsy and confused, his GCS declined from 15 to 12. However, the patient was still haemodynamically stable, as he had been in the morning. An arterial blood gas demonstrated a respiratory alkalosis (pH 7.55, pCO 2 3.1, pO 2 6.7 and HCO 3 24.9, lactate 1.8, base excess 0.5). He was commenced on intravenous co-amoxiclav and ciprofloxacin, to treat a potential exacerbation of COPD. This patient had a COVID-19 throat swab on 1 April 2020. Before the result of this swab, an early discussion was held with the intensive care unit staff, who decided at 17:00 on 1 April 2020 that given the patients presentation, rapid deterioration, comorbidities and likely COVID-19 diagnosis he would not be for escalation to the intensive care unit, and if he were to deteriorate further the end of life pathway would be most appropriate. The discussion was reiterated to the patients’ family, who were in agreement with this. Although he had evidence of an ischaemic stroke on CT of his brain, it was agreed by all clinicians that intervention for this was not as much of a priority as providing optimal palliative care, therefore, a minimally invasive method of treatment was advocated by the stroke team. The patient was given 300 mg of aspirin and was not a candidate for fibrinolysis.
Outcome and follow-up
The following day, before the throat swab result, had appeared the patient deteriorated further, requiring 15 L of oxygen through a non-rebreather face mask at 60% FiO 2 to maintain his oxygen saturation, at a maximum of 88% overnight. At this point, he was unresponsive to voice, with a GCS of 5. Although, he was still haemodynamically stable, with a blood pressure of 126/74 mm Hg and a heart rate of 98 beats/min. His respiratory rate was 30 breaths/min. His worsening respiratory condition, combined with his declining level of consciousness made it impossible to clinically assess progression of the neurological deficit generated by his cerebral infarction. Moreover, the patient was declining sharply while receiving the maximal ward-based treatment available. The senior respiratory physician overseeing the patients’ care decided that a palliative approach was in this his best interest, which was agreed on by all parties. The respiratory team completed the ‘recognising dying’ documentation, which signified that priorities of care had shifted from curative treatment to palliative care. Although the palliative team was not formally involved in the care of the patient, the patient received comfort measures without further attempts at supporting oxygenation, or conduction of regular clinical observations. The COVID-19 throat swab confirmed a positive result on 2 April 2020. The patient was treated by the medical team under jurisdiction of the hospital palliative care team. This included the prescribing of anticipatory medications and a syringe driver, which was established on 3 April 2020. His antibiotic treatment, non-essential medication and intravenous fluid treatment were discontinued. His comatose condition persisted throughout the admission. Once the patients’ GCS was 5, it did not improve. The patient was pronounced dead by doctors at 08:40 on 5 April 2020.
SARS-CoV-2 is a type of coronavirus that was first reported to have caused pneumonia-like infection in humans on 3 December 2019. 5 As a group, coronaviruses are a common cause of upper and lower respiratory tract infections (especially in children) and have been researched extensively since they were first characterised in the 1960s. 6 To date, there are seven coronaviruses that are known to cause infection in humans, including SARS-CoV-1, the first known zoonotic coronavirus outbreak in November 2002. 7 Coronavirus infections pass through communities during the winter months, causing small outbreaks in local communities, that do not cause significant mortality or morbidity.
SARS-CoV-2 strain of coronavirus is classed as a zoonotic coronavirus, meaning the virus pathogen is transmitted from non-humans to cause disease in humans. However the rapid spread of SARS-CoV-2 indicates human to human transmission is present. From previous research on the transmission of coronaviruses and that of SARS-CoV-2 it can be inferred that SARS-CoV-2 spreads via respiratory droplets, either from direct inhalation, or indirectly touching surfaces with the virus and exposing the eyes, nose or mouth. 8 Common signs and symptoms of the COVID-19 infection identified in patients include high fevers, severe fatigue, dry cough, acute breathing difficulties, bilateral pneumonia on radiological imaging and lymphopaenia. 9 Most of these features were identified in this case study. The significance of COVID-19 is illustrated by the speed of its global spread and the potential to cause severe clinical presentations, which as of April 2020 can only be treated symptomatically. In Italy, as of mid-March 2020, it was reported that 12% of the entire COVID-19 positive population and 16% of all hospitalised patients had an admission to the intensive care unit. 10
The patient, in this case, illustrates the clinical relevance of understanding COVID-19, as he presented with an ischaemic stroke underlined by minimal respiratory symptoms, which progressed expeditiously, resulting in acute respiratory distress syndrome and subsequent death.
Our case is an example of a new and ever-evolving clinical correlation, between patients who present with a radiological confirmed ischaemic stroke and severe COVID-19 pneumonia. As of April 2020, no comprehensive data of the relationship between ischaemic stroke and COVID-19 has been published, however early retrospective case series from three hospitals in Wuhan, China have indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke. 11 These studies have not yet undergone peer review, but they tell us a great deal about the relationship between COVID-19 and ischaemic stroke, and have been used to influence the American Heart Associations ‘Temporary Emergency Guidance to US Stroke Centres During the COVID-19 Pandemic’. 12
The relationship between similar coronaviruses and other viruses, such as influenza in the development of ischaemic stroke has previously been researched and provide a basis for further investigation, into the prominence of COVID-19 and its relation to ischaemic stroke. 3 Studies of SARS-CoV-2 indicate its receptor-binding region for entry into the host cell is the same as ACE2, which is present on endothelial cells throughout the body. It may be the case that SARS-CoV-2 alters the conventional ability of ACE2 to protect endothelial function in blood vessels, promoting atherosclerotic plaque displacement by producing an inflammatory response, thus increasing the risk of ischaemic stroke development. 13
Other hypothesised reasons for stroke development in COVID-19 patients are the development of hypercoagulability, as a result of critical illness or new onset of arrhythmias, caused by severe infection. Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer. Raised D-dimers are a non-specific marker of a prothrombotic state and have been associated with greater morbidity and mortality relating to stroke and other neurological features. 14
Arrhythmias such as atrial fibrillation had been identified in 17% of 138 COVID-19 patients, in a study conducted in Wuhan, China. 15 In this report, the patient was known to have atrial fibrillation and was treated with rivaroxaban. The acute inflammatory state COVID-19 is known to produce had the potential to create a prothrombotic environment, culminating in an ischaemic stroke.
Some early case studies produced in Wuhan describe patients in the sixth decade of life that had not been previously noted to have antiphospholipid antibodies, contain the antibodies in blood results. They are antibodies signify antiphospholipid syndrome; a prothrombotic condition. 16 This raises the hypothesis concerning the ability of COVID-19 to evoke the creation of these antibodies and potentiate thrombotic events, such as ischaemic stroke.
No peer-reviewed studies on the effects of COVID-19 and mechanism of stroke are published as of April 2020; therefore, it is difficult to evidence a specific reason as to why COVID-19 patients are developing neurological signs. It is suspected that a mixture of the factors mentioned above influence the development of ischaemic stroke.
If we delve further into this patients’ comorbid state exclusive to COVID-19 infection, it can be argued that this patient was already at a relatively higher risk of stroke development compared with the general population. The fact this patient had previously had an ischaemic stroke illustrates a prior susceptibility. This patient had a known background of hypertension and atrial fibrillation, which as mentioned previously, can influence blood clot or plaque propagation in the development of an acute ischaemic event. 15 Although the patient was prescribed rivaroxaban as an anticoagulant, true consistent compliance to rivaroxaban or other medications such as amlodipine, clopidogrel, candesartan and atorvastatin cannot be confirmed; all of which can contribute to the reduction of influential factors in the development of ischaemic stroke. Furthermore, the fear of contracting COVID-19, in addition to his vague symptoms, unlike his prior ischaemic stroke, which demonstrated dense left-sided haemiparesis, led to a delay in presentation to hospital. This made treatment options like fibrinolysis unachievable, although it can be argued that if he was already infected with COVID-19, he would have still developed life-threatening COVID-19 pneumonia, regardless of whether he underwent fibrinolysis. It is therefore important to consider that if this patient did not contract COVID-19 pneumonia, he still had many risk factors that made him prone to ischaemic stroke formation. Thus, we must consider whether similar patients would suffer from ischaemic stroke, regardless of COVID-19 infection and whether COVID-19 impacts on the severity of the stroke as an entity.
Having said this, the management of these patients is dependent on the likelihood of a positive outcome from the COVID-19 infection. Establishing the ceiling of care is crucial, as it prevents incredibly unwell or unfit patients’ from going through futile treatments, ensuring respect and dignity in death, if this is the likely outcome. It also allows for the provision of limited or intensive resources, such as intensive care beds or endotracheal intubation during the COVID-19 pandemic, to those who are assessed by the multidisciplinary team to benefit the most from their use. The way to establish this ceiling of care is through an early multidisciplinary discussion. In this case, the patient did not convey his wishes regarding his care to the medical team or his family; therefore it was decided among intensive care specialists, respiratory physicians, stroke physicians and the patients’ relatives. The patient was discussed with the intensive care team, who decided that as the patient sustained two acute life-threatening illnesses simultaneously and had rapidly deteriorated, ward-based care with a view to palliate if the further deterioration was in the patients’ best interests. These decisions were not easy to make, especially as it was on the first day of presentation. This decision was made in the context of the patients’ comorbidities, including COPD, the patients’ age, and the availability of intensive care beds during the steep rise in intensive care admissions, in the midst of the COVID-19 pandemic ( figure 1 ). Furthermore, the patients’ rapid and permanent decline in GCS, entwined with the severe stroke on CT imaging of the brain made it more unlikely that significant and permanent recovery could be achieved from mechanical intubation, especially as the damage caused by the stroke could not be significantly reversed. As hospitals manage patients with COVID-19 in many parts of the world, there may be tension between the need to provide higher levels of care for an individual patient and the need to preserve finite resources to maximise the benefits for most patients. This patient presented during a steep rise in intensive care admissions, which may have influenced the early decision not to treat the patient in an intensive care setting. Retrospective studies from Wuhan investigating mortality in patients with multiple organ failure, in the setting of COVID-19, requiring intubation have demonstrated mortality can be up to 61.5%. 17 The mortality risk is even higher in those over 65 years of age with respiratory comorbidities, indicating why this patient was unlikely to survive an admission to the intensive care unit. 18
Regularly updating the patients’ family ensured cooperation, empathy and sympathy. The patients’ stroke was not seen as a priority given the severity of his COVID-19 pneumonia, therefore the least invasive, but most appropriate treatment was provided for his stroke. The British Association of Stroke Physicians advocate this approach and also request the notification to their organisation of COVID-19-related stroke cases, in the UK. 19
Learning points
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is one of seven known coronaviruses that commonly cause upper and lower respiratory tract infections. It is the cause of the 2019–2020 global coronavirus pandemic.
The significance of COVID-19 is illustrated by the rapid speed of its spread globally and the potential to cause severe clinical presentations, such as ischaemic stroke.
Early retrospective data has indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke.
Potential mechanisms behind stroke in COVID-19 patients include a plethora of hypercoagulability secondary to critical illness and systemic inflammation, the development of arrhythmia, alteration to the vascular endothelium resulting in atherosclerotic plaque displacement and dehydration.
It is vital that effective, open communication between the multidisciplinary team, patient and patients relatives is conducted early in order to firmly establish the most appropriate ceiling of care for the patient.
- Cannine M , et al
- Wunderink RG
- van Doremalen N ,
- Bushmaker T ,
- Morris DH , et al
- Wang X-G , et al
- Grasselli G ,
- Pesenti A ,
- Wang M , et al
- American Stroke Assocation, 2020
- Zhang Y-H ,
- Zhang Y-huan ,
- Dong X-F , et al
- Li X , et al
- Hu C , et al
- Zhang S , et al
- Jiang B , et al
- Xu J , et al
- British Association of Stroke Physicians
Contributors SB was involved in the collecting of information for the case, the initial written draft of the case and researching existing data on acute stroke and COVID-19. He also edited drafts of the report. MH was involved in reviewing and editing drafts of the report and contributing new data. SP oversaw the conduction of the project and contributed addition research papers.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Next of kin consent obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:

Subscribe or Renew
Create an E-mail Alert for This Article
Case 6-2023: a 68-year-old man with recurrent strokes, permissions, information & authors, metrics & citations, continue reading this article.
Select an option below:
Create your account to get 2 free subscriber-only articles each month.
Already have an account, print subscriber, supplementary material, information, published in, translation.
- Clinical Medicine General
- Emergency Medicine General
- Hospital-Based Clinical Medicine
- Neurology/Neurosurgery General
- Outpatient-Based Clinical Medicine
- Rheumatology General
- Stroke (Emergency Medicine)
- Stroke (Neurology/Neurosurgery)
Affiliations
Export citation.
Select the format you want to export the citation of this publication.
- Igor Gomes Padilha,
- Ahmad Nehme,
- Hubert de Boysson,
- Laurent Létourneau-Guillon,
View Options
View options, content link.
Copying failed.
PREVIOUS ARTICLE
Next article, create your account for 2 free subscriber-only articles each month. get free access now..
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Neurotherapy for stroke rehabilitation: A single case study

1995, Biofeedback and Self-Regulation
Related Papers
Basic and Clinical Neuroscience Journal
Introduction: Depression is a mental disorder that highly associated with immune system. Therefore, this study compares the serum concentrations of IL-21, IL-17, and transforming growth factor β (TGF-β) between patients with major depressive disorder and healthy controls. Methods: Blood samples were collected from 41 patients with major depressive disorder and 40 healthy age-matched controls with no history of malignancies or autoimmune disorders. The subjects were interviewed face to face according to DSM-IV diagnostic criteria. Depression score was measured using completed Beck Depression Inventory in both groups. The serum concentrations of IL-21, IL-17, and TGF-β were assessed using ELISA. Results: The mean score of Beck Depression score in the patient and control groups was 35.4±5.5 and 11.1±2.3. IL-17 serum concentrations in the patients and the control group were 10.03±0.6 and 7.6±0.6 pg/mL, respectively (P=0.0002). TGF-β level in the patients group was significantly higher than compare to the control group; 336.7±20.19 vs. 174.8±27.20 pg/mL, (P<0.0001). However, the level of IL-21 was not statistically different between the two groups 84.30±4.57 vs. 84.12±4.15 pg/mL (P>0.05). Conclusion: Considering pro-inflammatory cytokines, current results support the association of inflammatory response and depressive disorder. So, it seems that pro-inflammatory factors profile can be used as indicator in following of depression progress and its treatment impacts.
Neurofeedback and Neuromodulation Techniques and Applications
Gabriel Tan
Applied Psychophysiology and Biofeedback
kirtley thornton
The onset of cognitive rehabilitation brought with it a hope for an effective treatment for the traumatic brain injured subject. This paper reviews the empirical reports of changes in cognitive functioning after treatment and compares the relative effectiveness of several treatments including computer interventions, cognitive strategies, EEG biofeedback, and medications. The cognitive functions that are reviewed include auditory memory, attention and problem solving. The significance of the change in cognitive function is assessed in two ways that include effect size and longevity of effect. These analyses complement the previously published meta-reviews by adding these two criteria and include reports of EEG biofeedback, which is shown to be an effective intervention for auditory memory.
Journal of Neurotherapy
Leslie Sherlin
John gruzelier
Introduction to Quantitative EEG and Neurofeedback
Victoria L. Ibric , Liviu Dragomirescu
Child and Adolescent Psychiatric Clinics of North America
NeuroRegulation
Journal of Clinical Psychology
Horst Mueller
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Seminars in Pediatric Neurology
Siegfried Othmer
Mahnaz Moghanloo
Ayben Ertem
Marco Congedo , Jan de Moor
Carlos Novo
Marvin W Sams
Malu Mascarenhas de Matos
Jeff La Marca
David Trudeau
Joshua Baruth , Ayman El-baz
Dennis Carmody
BRAIN. Broad Research in Artificial Intelligence and Neuroscience ISSN 2067-3957
Academia EduSoft
Dave Siever
Arnaud Delorme
Applied psychophysiology and biofeedback
Annals of the New York Academy of Sciences
Lewis Opler , Paul Ramirez
Autism Spectrum Disorders - From Genes to Environment
Jan de Moor
BMC Psychiatry
Irene Elgen , N. Duric
fateme dehghani arani
Journal of Alzheimer's disease : JAD
Marbella Espino
Child and Adolescent Psychiatric Clinics of North America - CHILD ADOLESC PSYCHIATR CLIN
Http Dx Doi Org 10 1300 J184v08n02_03
Research in Autism Spectrum Disorders
Michael Datko
Dave Siever , -Dave Siever
George Lindenfeld , John Hummer , James C Miller
Ann N Y Acad Sci
Paul Ramirez
Efthymios Angelakis , Joel Lubar
Meng Yie V Si Toh
Journal of …
David Trudeau , Joel Lubar , Robert Gurnee , Robert Thatcher
Neuropsychiatric disease and treatment
Saroja Krishnaswamy , Jamaludin Mohamed
Dove Medical Press
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

🎁🎄❄️ 50% Off Sale! ❄️ 🎄🎁
🌞🏝️😎 24 hours left to save 50% off our courses 😎 🏝️🌞, 😎 🏝️🌞 24 hours left to save 50% off our courses 😎 🏝️🌞, ❄️ 50% off holiday sale ❄️, emotional freedom techniques for stroke rehabilitation: a single case study.
Citation (APA style): Fuller, S. A., & Stapleton, P. (2021). Emotional Freedom Techniques for Stroke Rehabilitation: A Single Case Study. OBM Integrative and Complementary Medicine, 6 (4), 1-1.
Stroke, emotional freedom technique, tapping, guided imagery, visualization, cerebral, single case, depression, anxiety, trauma

Emotional Freedom Techniques or “EFT Tapping” is a powerful self-help method based on research showing that emotional trauma compromises both physical and emotional health.
Customer Support: +1 (877) 461-4026 Email
Subscribe to Our Newsletter
We value your privacy and never share your information. Includes free subscription to our awesome newsletter and promotional e-list and you agree to our terms of use and privacy policy .
Legal | Terms of Use | Privacy Policy | Testimonials And Results Disclosure | Affiliate Disclosure | Earnings Disclaimer
Emotional Freedom Techniques for Stroke Rehabilitation: A Single Case Study
- This person is not on ResearchGate, or hasn't claimed this research yet.

- Bond University
Abstract and Figures

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- Ann-Charlotte Laska

- Hayley Maree O’Neill

- Aytul Cakci
- Marit Kirkevold
- Line Kildal Bragstad

- John McLeod
- BBA-MOL BASIS DIS

- Alberto Zaliani
- Paola Baiardi

- Joyce A Kootker

- Frederik C. Lem

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 7: 10 Real Cases on Transient Ischemic Attack and Stroke: Diagnosis, Management, and Follow-Up
Jeirym Miranda; Fareeha S. Alavi; Muhammad Saad
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion, clinical symptoms.
- Radiologic Findings
- Full Chapter
- Supplementary Content
Case 1: Management of Acute Thrombotic Cerebrovascular Accident Post Recombinant Tissue Plasminogen Activator Therapy
A 59-year-old Hispanic man presented with right upper and lower extremity weakness, associated with facial drop and slurred speech starting 2 hours before the presentation. He denied visual disturbance, headache, chest pain, palpitations, dyspnea, dysphagia, fever, dizziness, loss of consciousness, bowel or urinary incontinence, or trauma. His medical history was significant for uncontrolled type 2 diabetes mellitus, hypertension, hyperlipidemia, and benign prostatic hypertrophy. Social history included cigarette smoking (1 pack per day for 20 years) and alcohol intake of 3 to 4 beers daily. Family history was not significant, and he did not remember his medications. In the emergency department, his vital signs were stable. His physical examination was remarkable for right-sided facial droop, dysarthria, and right-sided hemiplegia. The rest of the examination findings were insignificant. His National Institutes of Health Stroke Scale (NIHSS) score was calculated as 7. Initial CT angiogram of head and neck reported no acute intracranial findings. The neurology team was consulted, and intravenous recombinant tissue plasminogen activator (t-PA) was administered along with high-intensity statin therapy. The patient was admitted to the intensive care unit where his hemodynamics were monitored for 24 hours and later transferred to the telemetry unit. MRI of the head revealed an acute 1.7-cm infarct of the left periventricular white matter and posterior left basal ganglia. How would you manage this case?
This case scenario presents a patient with acute ischemic cerebrovascular accident (CVA) requiring intravenous t-PA. Diagnosis was based on clinical neurologic symptoms and an NIHSS score of 7 and was later confirmed by neuroimaging. He had multiple comorbidities, including hypertension, diabetes, dyslipidemia, and smoking history, which put him at a higher risk for developing cardiovascular disease. Because his symptoms started within 4.5 hours of presentation, he was deemed to be a candidate for thrombolytics. The eligibility time line is estimated either by self-report or last witness of baseline status.
Ischemic strokes are caused by an obstruction of a blood vessel, which irrigates the brain mainly secondary to the development of atherosclerotic changes, leading to cerebral thrombosis and embolism. Diagnosis is made based on presenting symptoms and CT/MRI of the head, and the treatment is focused on cerebral reperfusion based on eligibility criteria and timing of presentation.
Symptoms include alteration of sensorium, numbness, decreased motor strength, facial drop, dysarthria, ataxia, visual disturbance, dizziness, and headache.
Get Free Access Through Your Institution
Pop-up div successfully displayed.
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMJ Case Rep

Case report
Clinical course of a 66-year-old man with an acute ischaemic stroke in the setting of a covid-19 infection, saajan basi.
1 Department of Stroke and Acute Medicine, King's Mill Hospital, Sutton-in-Ashfield, UK
2 Department of Acute Medicine, University Hospitals of Derby and Burton, Derby, UK
Mohammad Hamdan
Shuja punekar.
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater oxygen requirement, alongside reduced levels of consciousness. A positive COVID-19 throat swab, in addition to bilateral pneumonia on chest X-ray and lymphopaenia in his blood tests, confirmed a diagnosis of COVID-19 pneumonia. A proactive decision was made involving the patients’ family, ward and intensive care healthcare staff, to not escalate care above a ward-based ceiling of care. The patient died 5 days following admission under the palliative care provided by the medical team.
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is a new strain of coronavirus that is thought to have originated in December 2019 in Wuhan, China. In a matter of months, it has erupted from non-existence to perhaps the greatest challenge to healthcare in modern times, grinding most societies globally to a sudden halt. Consequently, the study and research into SARS-CoV-2 is invaluable. Although coronaviruses are common, SARS-CoV-2 appears to be considerably more contagious. The WHO figures into the 2003 SARS-CoV-1 outbreak, from November 2002 to July 2003, indicate a total of 8439 confirmed cases globally. 1 In comparison, during a period of 4 months from December 2019 to July 2020, the number of global cases of COVID-19 reached 10 357 662, increasing exponentially, illustrating how much more contagious SARS-CoV-2 has been. 2
Previous literature has indicated infections, and influenza-like illness have been associated with an overall increase in the odds of stroke development. 3 There appears to be a growing correlation between COVID-19 positive patients presenting to hospital with ischaemic stroke; however, studies investigating this are in progress, with new data emerging daily. This patient report comments on and further characterises the link between COVID-19 pneumonia and the development of ischaemic stroke. At the time of this patients’ admission, there were 95 positive cases from 604 COVID-19 tests conducted in the local community, with a predicted population of 108 000. 4 Only 4 days later, when this patient died, the figure increased to 172 positive cases (81% increase), illustrating the rapid escalation towards the peak of the pandemic, and widespread transmission within the local community ( figure 1 ). As more cases of ischaemic stroke in COVID-19 pneumonia patients arise, the recognition and understanding of its presentation and aetiology can be deciphered. Considering the virulence of SARS-CoV-2 it is crucial as a global healthcare community, we develop this understanding, in order to intervene and reduce significant morbidity and mortality in stroke patients.

A graph showing the number of patients with COVID-19 in the hospital and in the community over time.
Case presentation
A 66-year-old man presented to the hospital with signs of left-sided weakness. The patient had a background of chronic obstructive pulmonary disease (COPD), atrial fibrillation and had one previous ischaemic stroke, producing left-sided haemiparesis, which had completely resolved. He was a non-smoker and lived in a house. The patient was found slumped over on the sofa at home on 1 April 2020, by a relative at approximately 01:00, having been seen to have no acute medical illness at 22:00. The patients’ relative initially described disorientation and agitation with weakness noted in the left upper limb and dysarthria. At the time of presentation, neither the patient nor his relative identified any history of fever, cough, shortness of breath, loss of taste, smell or any other symptoms; however, the patient did have a prior admission 9 days earlier with shortness of breath.
The vague nature of symptoms, entwined with considerable concern over approaching the hospital, due to the risk of contracting COVID-19, created a delay in the patients’ attendance to the accident and emergency department. His primary survey conducted at 09:20 on 1 April 2020 demonstrated a patent airway, with spontaneous breathing and good perfusion. His Glasgow Coma Scale (GCS) score was 15 (a score of 15 is the highest level of consciousness), his blood glucose was 7.2, and he did not exhibit any signs of trauma. His abbreviated mental test score was 7 out of 10, indicating a degree of altered cognition. An ECG demonstrated atrial fibrillation with a normal heart rate. His admission weight measured 107 kg. At 09:57 the patient required 2 L of nasal cannula oxygen to maintain his oxygen saturations between 88% and 92%. He started to develop agitation associated with an increased respiratory rate at 36 breaths per minute. On auscultation of his chest, he demonstrated widespread coarse crepitation and bilateral wheeze. Throughout he was haemodynamically stable, with a systolic blood pressure between 143 mm Hg and 144 mm Hg and heart rate between 86 beats/min and 95 beats/min. From a neurological standpoint, he had a mild left facial droop, 2/5 power in both lower limbs, 2/5 power in his left upper limb and 5/5 power in his right upper limb. Tone in his left upper limb had increased. This patient was suspected of having COVID-19 pneumonia alongside an ischaemic stroke.
Investigations
A CT of his brain conducted at 11:38 on 1 April 2020 ( figure 2 ) illustrated an ill-defined hypodensity in the right frontal lobe medially, with sulcal effacement and loss of grey-white matter. This was highly likely to represent acute anterior cerebral artery territory infarction. Furthermore an oval low-density area in the right cerebellar hemisphere, that was also suspicious of an acute infarction. These vascular territories did not entirely correlate with his clinical picture, as limb weakness is not as prominent in anterior cerebral artery territory ischaemia. Therefore this left-sided weakness may have been an amalgamation of residual weakness from his previous stroke, in addition to his acute cerebral infarction. An erect AP chest X-ray with portable equipment ( figure 3 ) conducted on the same day demonstrated patchy peripheral consolidation bilaterally, with no evidence of significant pleural effusion. The pattern of lung involvement raised suspicion of COVID-19 infection, which at this stage was thought to have provoked the acute cerebral infarct. Clinically significant blood results from 1 April 2020 demonstrated a raised C-reactive protein (CRP) at 215 mg/L (normal 0–5 mg/L) and lymphopaenia at 0.5×10 9 (normal 1×10 9 to 3×10 9 ). Other routine blood results are provided in table 1 .

CT imaging of this patients’ brain demonstrating a wedge-shaped infarction of the anterior cerebral artery territory.

Chest X-ray demonstrating the bilateral COVID-19 pneumonia of this patient on admission.
Clinical biochemistry and haematology blood results of the patient
| Hb | 157 g/L |
| WCC | 5.8 |
| Platelet count | 195 |
| MCV | 86 |
| Neutrophils | 4.9 |
| Lymphocytes | 0.5 |
| INR | 1.3 |
| PT | 16.7 |
| APTT | 28 |
| Sodium | 137 |
| Potassium | Sample haemolysed |
| Urea | 9.5 |
| Creatinine | 84 |
| eGFR | 83 |
| Bilirubin | 26 |
| Albumin | 29 |
| CRP | 215 |
| Total protein | 69 |
APTT, activated partial thromboplastin time; CRP, C-reactive protein; eGFR, estimated glomerular filtration rate; Hb, haemoglobin; INR, international normalised ratio; MCV, mean corpuscular volume; PT, prothrombin time; WCC, white cell count.
Interestingly the patient, in this case, was clinically assessed in the accident and emergency department on 23 March 2020, 9 days prior to admission, with symptoms of shortness of breath. His blood results from this day showed a CRP of 22 mg/L and a greater lymphopaenia at 0.3×10 9 . He had a chest X-ray ( figure 4 ), which indicated mild radiopacification in the left mid zone. He was initially treated with intravenous co-amoxiclav and ciprofloxacin. The following day he had minimal symptoms (CURB 65 score 1 for being over 65 years). Given improving blood results (declining CRP), he was discharged home with a course of oral amoxicillin and clarithromycin. As national governmental restrictions due to COVID-19 had not been formally announced until 23 March 2020, and inconsistencies regarding personal protective equipment training and usage existed during the earlier stages of this rapidly evolving pandemic, it is possible that this patient contracted COVID-19 within the local community, or during his prior hospital admission. It could be argued that the patient had early COVID-19 signs and symptoms, having presented with shortness of breath, lymphopaenia, and having had subtle infective chest X-ray changes. The patient explained he developed a stagnant productive cough, which began 5 days prior to his attendance to hospital on 23 March 2020. He responded to antibiotics, making a full recovery following 7 days of treatment. This information does not assimilate with the typical features of a COVID-19 infection. A diagnosis of community-acquired pneumonia or infective exacerbation of COPD seem more likely. However, given the high incidence of COVID-19 infections during this patients’ illness, an exposure and early COVID-19 illness, prior to the 23 March 2020, cannot be completely ruled out.

Chest X-ray conducted on prior admission illustrating mild radiopacification in the left mid zone.
On the current admission, this patient was managed with nasal cannula oxygen at 2 L. By the end of the day, this had progressed to a venturi mask, requiring 8 L of oxygen to maintain oxygen saturation. He had also become increasingly drowsy and confused, his GCS declined from 15 to 12. However, the patient was still haemodynamically stable, as he had been in the morning. An arterial blood gas demonstrated a respiratory alkalosis (pH 7.55, pCO 2 3.1, pO 2 6.7 and HCO 3 24.9, lactate 1.8, base excess 0.5). He was commenced on intravenous co-amoxiclav and ciprofloxacin, to treat a potential exacerbation of COPD. This patient had a COVID-19 throat swab on 1 April 2020. Before the result of this swab, an early discussion was held with the intensive care unit staff, who decided at 17:00 on 1 April 2020 that given the patients presentation, rapid deterioration, comorbidities and likely COVID-19 diagnosis he would not be for escalation to the intensive care unit, and if he were to deteriorate further the end of life pathway would be most appropriate. The discussion was reiterated to the patients’ family, who were in agreement with this. Although he had evidence of an ischaemic stroke on CT of his brain, it was agreed by all clinicians that intervention for this was not as much of a priority as providing optimal palliative care, therefore, a minimally invasive method of treatment was advocated by the stroke team. The patient was given 300 mg of aspirin and was not a candidate for fibrinolysis.
Outcome and follow-up
The following day, before the throat swab result, had appeared the patient deteriorated further, requiring 15 L of oxygen through a non-rebreather face mask at 60% FiO 2 to maintain his oxygen saturation, at a maximum of 88% overnight. At this point, he was unresponsive to voice, with a GCS of 5. Although, he was still haemodynamically stable, with a blood pressure of 126/74 mm Hg and a heart rate of 98 beats/min. His respiratory rate was 30 breaths/min. His worsening respiratory condition, combined with his declining level of consciousness made it impossible to clinically assess progression of the neurological deficit generated by his cerebral infarction. Moreover, the patient was declining sharply while receiving the maximal ward-based treatment available. The senior respiratory physician overseeing the patients’ care decided that a palliative approach was in this his best interest, which was agreed on by all parties. The respiratory team completed the ‘recognising dying’ documentation, which signified that priorities of care had shifted from curative treatment to palliative care. Although the palliative team was not formally involved in the care of the patient, the patient received comfort measures without further attempts at supporting oxygenation, or conduction of regular clinical observations. The COVID-19 throat swab confirmed a positive result on 2 April 2020. The patient was treated by the medical team under jurisdiction of the hospital palliative care team. This included the prescribing of anticipatory medications and a syringe driver, which was established on 3 April 2020. His antibiotic treatment, non-essential medication and intravenous fluid treatment were discontinued. His comatose condition persisted throughout the admission. Once the patients’ GCS was 5, it did not improve. The patient was pronounced dead by doctors at 08:40 on 5 April 2020.
SARS-CoV-2 is a type of coronavirus that was first reported to have caused pneumonia-like infection in humans on 3 December 2019. 5 As a group, coronaviruses are a common cause of upper and lower respiratory tract infections (especially in children) and have been researched extensively since they were first characterised in the 1960s. 6 To date, there are seven coronaviruses that are known to cause infection in humans, including SARS-CoV-1, the first known zoonotic coronavirus outbreak in November 2002. 7 Coronavirus infections pass through communities during the winter months, causing small outbreaks in local communities, that do not cause significant mortality or morbidity.
SARS-CoV-2 strain of coronavirus is classed as a zoonotic coronavirus, meaning the virus pathogen is transmitted from non-humans to cause disease in humans. However the rapid spread of SARS-CoV-2 indicates human to human transmission is present. From previous research on the transmission of coronaviruses and that of SARS-CoV-2 it can be inferred that SARS-CoV-2 spreads via respiratory droplets, either from direct inhalation, or indirectly touching surfaces with the virus and exposing the eyes, nose or mouth. 8 Common signs and symptoms of the COVID-19 infection identified in patients include high fevers, severe fatigue, dry cough, acute breathing difficulties, bilateral pneumonia on radiological imaging and lymphopaenia. 9 Most of these features were identified in this case study. The significance of COVID-19 is illustrated by the speed of its global spread and the potential to cause severe clinical presentations, which as of April 2020 can only be treated symptomatically. In Italy, as of mid-March 2020, it was reported that 12% of the entire COVID-19 positive population and 16% of all hospitalised patients had an admission to the intensive care unit. 10
The patient, in this case, illustrates the clinical relevance of understanding COVID-19, as he presented with an ischaemic stroke underlined by minimal respiratory symptoms, which progressed expeditiously, resulting in acute respiratory distress syndrome and subsequent death.
Our case is an example of a new and ever-evolving clinical correlation, between patients who present with a radiological confirmed ischaemic stroke and severe COVID-19 pneumonia. As of April 2020, no comprehensive data of the relationship between ischaemic stroke and COVID-19 has been published, however early retrospective case series from three hospitals in Wuhan, China have indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke. 11 These studies have not yet undergone peer review, but they tell us a great deal about the relationship between COVID-19 and ischaemic stroke, and have been used to influence the American Heart Associations ‘Temporary Emergency Guidance to US Stroke Centres During the COVID-19 Pandemic’. 12
The relationship between similar coronaviruses and other viruses, such as influenza in the development of ischaemic stroke has previously been researched and provide a basis for further investigation, into the prominence of COVID-19 and its relation to ischaemic stroke. 3 Studies of SARS-CoV-2 indicate its receptor-binding region for entry into the host cell is the same as ACE2, which is present on endothelial cells throughout the body. It may be the case that SARS-CoV-2 alters the conventional ability of ACE2 to protect endothelial function in blood vessels, promoting atherosclerotic plaque displacement by producing an inflammatory response, thus increasing the risk of ischaemic stroke development. 13
Other hypothesised reasons for stroke development in COVID-19 patients are the development of hypercoagulability, as a result of critical illness or new onset of arrhythmias, caused by severe infection. Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer. Raised D-dimers are a non-specific marker of a prothrombotic state and have been associated with greater morbidity and mortality relating to stroke and other neurological features. 14
Arrhythmias such as atrial fibrillation had been identified in 17% of 138 COVID-19 patients, in a study conducted in Wuhan, China. 15 In this report, the patient was known to have atrial fibrillation and was treated with rivaroxaban. The acute inflammatory state COVID-19 is known to produce had the potential to create a prothrombotic environment, culminating in an ischaemic stroke.
Some early case studies produced in Wuhan describe patients in the sixth decade of life that had not been previously noted to have antiphospholipid antibodies, contain the antibodies in blood results. They are antibodies signify antiphospholipid syndrome; a prothrombotic condition. 16 This raises the hypothesis concerning the ability of COVID-19 to evoke the creation of these antibodies and potentiate thrombotic events, such as ischaemic stroke.
No peer-reviewed studies on the effects of COVID-19 and mechanism of stroke are published as of April 2020; therefore, it is difficult to evidence a specific reason as to why COVID-19 patients are developing neurological signs. It is suspected that a mixture of the factors mentioned above influence the development of ischaemic stroke.
If we delve further into this patients’ comorbid state exclusive to COVID-19 infection, it can be argued that this patient was already at a relatively higher risk of stroke development compared with the general population. The fact this patient had previously had an ischaemic stroke illustrates a prior susceptibility. This patient had a known background of hypertension and atrial fibrillation, which as mentioned previously, can influence blood clot or plaque propagation in the development of an acute ischaemic event. 15 Although the patient was prescribed rivaroxaban as an anticoagulant, true consistent compliance to rivaroxaban or other medications such as amlodipine, clopidogrel, candesartan and atorvastatin cannot be confirmed; all of which can contribute to the reduction of influential factors in the development of ischaemic stroke. Furthermore, the fear of contracting COVID-19, in addition to his vague symptoms, unlike his prior ischaemic stroke, which demonstrated dense left-sided haemiparesis, led to a delay in presentation to hospital. This made treatment options like fibrinolysis unachievable, although it can be argued that if he was already infected with COVID-19, he would have still developed life-threatening COVID-19 pneumonia, regardless of whether he underwent fibrinolysis. It is therefore important to consider that if this patient did not contract COVID-19 pneumonia, he still had many risk factors that made him prone to ischaemic stroke formation. Thus, we must consider whether similar patients would suffer from ischaemic stroke, regardless of COVID-19 infection and whether COVID-19 impacts on the severity of the stroke as an entity.
Having said this, the management of these patients is dependent on the likelihood of a positive outcome from the COVID-19 infection. Establishing the ceiling of care is crucial, as it prevents incredibly unwell or unfit patients’ from going through futile treatments, ensuring respect and dignity in death, if this is the likely outcome. It also allows for the provision of limited or intensive resources, such as intensive care beds or endotracheal intubation during the COVID-19 pandemic, to those who are assessed by the multidisciplinary team to benefit the most from their use. The way to establish this ceiling of care is through an early multidisciplinary discussion. In this case, the patient did not convey his wishes regarding his care to the medical team or his family; therefore it was decided among intensive care specialists, respiratory physicians, stroke physicians and the patients’ relatives. The patient was discussed with the intensive care team, who decided that as the patient sustained two acute life-threatening illnesses simultaneously and had rapidly deteriorated, ward-based care with a view to palliate if the further deterioration was in the patients’ best interests. These decisions were not easy to make, especially as it was on the first day of presentation. This decision was made in the context of the patients’ comorbidities, including COPD, the patients’ age, and the availability of intensive care beds during the steep rise in intensive care admissions, in the midst of the COVID-19 pandemic ( figure 1 ). Furthermore, the patients’ rapid and permanent decline in GCS, entwined with the severe stroke on CT imaging of the brain made it more unlikely that significant and permanent recovery could be achieved from mechanical intubation, especially as the damage caused by the stroke could not be significantly reversed. As hospitals manage patients with COVID-19 in many parts of the world, there may be tension between the need to provide higher levels of care for an individual patient and the need to preserve finite resources to maximise the benefits for most patients. This patient presented during a steep rise in intensive care admissions, which may have influenced the early decision not to treat the patient in an intensive care setting. Retrospective studies from Wuhan investigating mortality in patients with multiple organ failure, in the setting of COVID-19, requiring intubation have demonstrated mortality can be up to 61.5%. 17 The mortality risk is even higher in those over 65 years of age with respiratory comorbidities, indicating why this patient was unlikely to survive an admission to the intensive care unit. 18
Regularly updating the patients’ family ensured cooperation, empathy and sympathy. The patients’ stroke was not seen as a priority given the severity of his COVID-19 pneumonia, therefore the least invasive, but most appropriate treatment was provided for his stroke. The British Association of Stroke Physicians advocate this approach and also request the notification to their organisation of COVID-19-related stroke cases, in the UK. 19
Learning points
- SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) is one of seven known coronaviruses that commonly cause upper and lower respiratory tract infections. It is the cause of the 2019–2020 global coronavirus pandemic.
- The significance of COVID-19 is illustrated by the rapid speed of its spread globally and the potential to cause severe clinical presentations, such as ischaemic stroke.
- Early retrospective data has indicated that up to 36% of COVID-19 patients had neurological manifestations, including stroke.
- Potential mechanisms behind stroke in COVID-19 patients include a plethora of hypercoagulability secondary to critical illness and systemic inflammation, the development of arrhythmia, alteration to the vascular endothelium resulting in atherosclerotic plaque displacement and dehydration.
- It is vital that effective, open communication between the multidisciplinary team, patient and patients relatives is conducted early in order to firmly establish the most appropriate ceiling of care for the patient.
Contributors: SB was involved in the collecting of information for the case, the initial written draft of the case and researching existing data on acute stroke and COVID-19. He also edited drafts of the report. MH was involved in reviewing and editing drafts of the report and contributing new data. SP oversaw the conduction of the project and contributed addition research papers.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Next of kin consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
- Open access
- Published: 09 September 2024
Stroke after heart valve surgery: a single center institution report
- Nizar Alwaqfi 1 ,
- Majd M. AlBarakat 1 ,
- Hala Qariouti 1 ,
- Khalid Ibrahim 1 &
- Nabil alzoubi 1
Journal of Cardiothoracic Surgery volume 19 , Article number: 518 ( 2024 ) Cite this article
1 Altmetric
Metrics details
Introduction
Stroke is a potentially debilitating complication of heart valve replacement surgery, with rates ranging from 1 to 10%. Despite advancements in surgical techniques, the incidence of postoperative stroke remains a significant concern, impacting patient outcomes and healthcare resources. This study aims to investigate the incidence, risk factors, and outcomes of in-hospital adverse neurologic events, particularly stroke, following valve replacement. The analysis focuses on identifying patient characteristics and procedural factors associated with increased stroke risk.
This retrospective study involves a review of 417 consecutive patients who underwent SVR between January 2004 and December 2022. The study cohort was extracted from a prospectively recorded cardiac intensive care unit database. Preoperative and perioperative data were collected, and subjects with specific exclusion criteria were omitted from the analysis. The analysis includes demographic information, preoperative risk factors, and perioperative variables.
The study identified a 4.3% incidence of postoperative stroke among SVR patients. Risk factors associated with increased stroke susceptibility included prolonged cardiopulmonary bypass time, aortic cross-clamp duration exceeding 90 min, prior stroke history, diabetes mellitus, and mitral valve annulus calcification. Patients undergoing combined procedures, such as aortic valve replacement with mitral valve replacement or coronary artery bypass grafting with AVR and MVR, (OR = 10.74, CI:2.65–43.44, p-value = < 0.001) and (OR = 11.66, CI:1.02–132.70, p-value = 0.048) respectively, exhibited elevated risks. Internal carotid artery stenosis (< 75%) and requiring prolonged inotropic support were also associated with increased stroke risk(OR = 3.04, CI:1.13–8.12, P-value = 0.026). The occurrence of stroke correlated with extended intensive care unit stay (OR = 1.12, CI: 1.04–1.20, P-value = 0.002) and heightened in-hospital mortality.
In conclusion, our study identifies key risk factors and underscores the importance of proactive measures to reduce postoperative stroke incidence in surgical valve replacement patients.
Peer Review reports
Stroke is a rare but still a potentially crippling complication of heart valve replacement surgery with risk dependent on patient characteristics and concomitant procedures. Stroke rates after surgical valve replacement (SVR) have ranged widely from 1 to 10% [ 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 ].
Studies of clinical stroke-complicating cardiac surgeries have reported increased duration and cost of hospitalization, dramatically elevated in-hospital mortality, and a high rate of severe disability in survivors [ 4 , 8 , 9 ].
Several studies have evaluated risk factors and postoperative neurologic complications after heart valve surgery, though the results are conflicting or incomplete mainly due to a low number of interventions or a low number of variables. Also, the low incidence of this postoperative key event limits the power of most published papers. Some studies have reported the association between prolonged cardiopulmonary bypass (CPB) and the development of postoperative stroke, while others have questioned its significance [ 11 , 12 , 13 , 14 ]. Other reported risk factors include age, concomitant atrial fibrillation (AF), history of cerebrovascular (CV) disease, concomitant carotid artery (CA) stenosis and aortic atherosclerosis, preoperative left ventricular (LV) dysfunction, concomitant procedures and lack of postoperative anticoagulation. [ 10 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 ] Recently, there is evidence that the rate of neurologic complications after SVR has been increasing, likely because of the willingness of surgeons to operate on older and higher-risk patients. [ 1 , 16 ] As such the current literature provides heterogeneous rates of adverse in-hospital neurologic complications after SVR. This heterogeneity, especially from the clinical trials, has raised the issue of whether the real-life stroke rate after heart valve surgery is different from that in the trial setting.
To address this issue and to the best of our knowledge, in our institution, stroke incidence, risk factors, and outcomes were not reported. We aimed to assess the incidence of in-hospital adverse neurologic events after SVR (with or without coronary artery bypass grafting [CABG]) and to identify patient and disease factors associated with stroke. In addition, the impact of postoperative stroke on length of hospital stay (LOS) and in-hospital mortality was evaluated.
Materials and methods
This study is a retrospective review of the clinical, operative, and outcome data that is part of the prospectively recorded cardiac intensive care unit (CICU) database. The present analysis includes all replacement valve surgeries performed between January 2004 and December 2022. Preoperative and perioperative data were retrospectively collected. After isolation of data, subjects were excluded if they had undergone CA stenting or endarterectomy within the previous 6 weeks; had any significant neurological disease, defined as the incidence of stroke or transient ischemic attack (TIA) within the preceding 6 months; had symptomatic or asymptomatic severe occlusive CA disease requiring concomitant endarterectomy/stenting. Also, patients who underwent valve repair, additional procedures on the aorta, and redo valve surgery were excluded from the study. Additionally, patients were excluded if an additional surgical procedure on the ascending aorta was performed.
The studied population consisted of 417 consecutive patients. Two groups were identified; Group 1 consisted of 18 patients who had a postoperative stroke, and group 2 consisted of the remaining patients (399) in the cohort. This work was approved by the ethical committee in the institution and the patient`s signature was waived.
Preoperative data
Patient’s medical records were reviewed for prior stroke; results of brain computerized tomography (CT) scan or magnetic resonance imaging (MRI), when available, or presence of unresolved neurological deficit, body mass index (BMI), New York Heart Association (NYHA) classification; symptomatic patients or on anti-failure treatment, diabetes mellitus (DM); with the majority being type 2 diabetes managed with oral hypoglycemic agents, hypertension; previously diagnosed and on anti-hypertensive treatment, chronic renal impairment (CRI); creatinine ≥ 1.5 mg/dl or on chronic dialysis, peripheral vascular disease (PVD); positive history of intermittent claudication or a documented clinical evidence of peripheral ischemia, left ventricular ejection fraction (LVEF); by either angiography or echocardiography, number of diseased coronary arteries; based on coronary angiogram and operative reports.
CA duplex scanning or CT scan angiography was performed routinely for most of the patients (80% of the studied cohort); almost 8% had severe CA stenosis (luminal narrowing ≥ 75%) and 24.5% had moderate disease. Patients with severe CA stenosis were sent for surgical or percutaneous intervention before valve surgery.
Perioperative antithrombotic treatment
Patients who were taking aspirin (100 mg) continued this medication without interruption preoperatively. Heparin (3.0 mg/kg) was administered intravenously before cardiopulmonary bypass (CPB) to maintain an activated clotting time (ACT) greater than 400 s. At the end of the procedure, heparin was neutralized with protamine sulfate (3.0 mg/kg). Additional protamine was administered if ACT remained above 140 s before chest closure. Neither aprotinin nor tranexamic acid was used in any patient. Transfusion of packed red blood cells, fresh frozen plasma, and platelets was determined based on bleeding volume, International Normalized Ratio (INR) levels, and platelet counts.
Postoperatively, patients received warfarin with bridging using unfractionated heparin or enoxaparin until the INR reached therapeutic levels. The target INR was 2.5 to 3 times normal for patients with St. Jude, Carbomedics, or Medtronic Hall aortic valves, and 3 to 3.5 times normal for patients with St. Jude, Carbomedics, or Medtronic Hall mitral valves. Patients with more than one prosthetic valve were maintained at a target INR of 3.5 to 4 times normal. The addition of daily aspirin (100 mg) was at the discretion of the treating physician.
Patients with bioprosthetic valves received warfarin for 1 to 3 months postoperatively, followed by lifelong aspirin therapy. In patients with bioprosthetic valves and atrial fibrillation, warfarin was continued as clinically indicated.
Intraoperative data
Assessment of the ascending aorta was performed using digital palpation. It is noted that none of the stroke patients included in this study had documented atherosclerotic disease of the ascending aorta; therefore, this variable was not specifically assessed.
Standard techniques were employed for cardiopulmonary bypass (CPB), ensuring perfusion was maintained at 2.0 to 2.4 L/min/m². Systemic perfusion pressure was carefully regulated within the range of 60 to 80 mmHg throughout the procedure. Myocardial viability was preserved through the use of cold antegrade potassium cardioplegia and topical hypothermia techniques. Furthermore, body temperature was meticulously controlled and maintained between 28 °C and 32 °C to optimize surgical conditions and patient outcomes.
Neurological complications
Stroke was defined as any new focal neurological dysfunction of presumed vascular origin lasting more than 24 h. A neurological assessment is routinely done by the surgical team if patients are extubated within 24 h. Patients with positive neurological examination, suspected neurological deficit, and/or prolonged time on ventilator are usually assessed by the neurologists. Stroke diagnosis was based on clinical findings and brain imaging by CT scan or MRI.
Statistical analysis
Continuous variables are presented as either mean ± standard deviation or median [interquartile range], depending on the distribution normality. Categorical variables are displayed as counts (percentages). Odds ratios (OR) and 95% confidence intervals (CI) were calculated for categorical data comparisons. A p-value of less than 0.05 was deemed statistically significant. All statistical analyses were conducted using R software (version 3.4.0, R Foundation, Vienna, Austria).
Table 1 displays the demographics and univariate analyses of patient characteristics in groups 1 (stroke) and 2 (no stroke). There were 17 (4.3%) patients in group 1 and 399 patients in group 2. The average age for group 1 was 59.5 (± 9.44) years, whereas for group 2 it was 51.6 (± 15.3) years, yielding a statistically significant difference ( p = 0.003). The mean BMI for group 1 was 28.8 (± 4.36), while for group 2 it was 22.0 (± 5.1%).
Approximately 44.4% of patients in the postoperative stroke group exhibited mitral valve annulus calcification (MVAC), whereas this figure was only 17% in the other group. Additionally, 50% of the patients with stroke had DM, in contrast to only 20% in the other group. The most prevalent type of operation in the stroke group was AVR combined with MVR, whereas in the other group, AVR alone was the predominant procedure.
Table 2 . presents the Crude Odds Ratios (OR) and their corresponding 95% Confidence Intervals (CI) for factors associated with postoperative Stroke. Patients undergoing procedures such as AVR with MVR, MVR with CABG, and AVR with MVR and CABG exhibited elevated risks of postoperative stroke, with odds ratios of 10, 5, and 11 respectively.
Patients with internal CA stenosis ranging from 50% to less than 75% demonstrated a substantially increased susceptibility to stroke, with an odds ratio of 4.129 (CI: 1.3887–12.2761) and a p-value of 0.011. Similarly, individuals with DM were associated with a heightened risk, displaying an odds ratio of 3.9259 (CI: 1.5098–10.2082) and a p-value of 0.005.
Patients with a prior history of stroke exhibited a higher risk with an odds ratio of 4.4643 and a CI of (1.3645–14.6064), with a p-value of 0.013. Furthermore, CPB exceeding 120 min demonstrated a significantly elevated risk in comparison to durations less than 120 min, with an odds ratio of 6.312 and a CI of 0.4631–9.9076 ( p < 0.001). Additionally, aortic cross-clamping for more than 90 min demonstrated a heightened risk with an odds ratio of 6.2661 and a CI of 2.3546–16.6754, with a p-value less than 0.001.
Patients requiring prolonged inotropic support for more than 48 h demonstrated a significantly increased risk, with an odds ratio of 3.04 (95% CI: 1.14–8.13) and a p-value of 0.026. Furthermore, the occurrence of stroke was associated with an extended stay in the CICU, indicated by an odds ratio of 1.12 (95% CI: 1.04–1.20) and a p-value of 0.002.
The stroke group exhibited a significantly elevated postoperative mortality risk, with an OR of 7.05 (95% confidence interval [CI]: 1.78–27.95), indicating a substantial increase in risk. The corresponding p-value was 0.005.
In our study, we assessed the occurrence of postoperative stroke in 417 consecutive SVR patients which included different valve replacement and combined surgeries. We found that 4.3% of patients experienced postoperative stroke, matching what was reported by Raffa et al. [ 23 ] with a sample size of 2121 patients. This drastic complication was significantly associated with prolonged CICU stay and increased operative mortality, this association was clearly established in our analysis, underscoring the importance of identifying potential risk factors to mitigate postoperative neurological complications. The exact reason for this high mortality associated with stroke remains unclear. We think most of stroke patients are elderly with multiple comorbidities, spend long time in CICU on ventilator, which make them prone for major complications, particularly respiratory failure and sepsis. [ 10 , 18 ]
The etiology of postoperative stroke after cardiac surgery is multifactorial, with embolism being the predominant cause, while intraoperative hypotension and hemorrhage are less common. [ 24 ] Most of our patients had a stroke, however, we couldn’t identify embolization or perioperative hypotension as the possible cause. Also, nothing was mentioned in most of the operative notes about the status of the ascending aorta; this may be related to the observed negligible incidence of atherosclerotic changes of the ascending aorta in our patients, which is the major source of emboli to the brain.
In our study having a unilateral ICA stenosis (< 75%) was significantly associated with an increased risk of stroke, which may be necisating further preoperative assessment of the extracardiac arterial system.
Our analysis indicated that a history of prior stroke was a robust preoperative predictor of stroke, with an OR of approximately 4.5. A history of stroke may indicate underlying pathological conditions within the cerebrovascular arteries. Bucerius et al. [ 10 ] conducted a similar study involving 16,184 patients and reported a stroke incidence of 16.8% in patients with cerebrovascular disease undergoing similar surgeries. In our study, the incidence was even higher, with our analysis revealing that 22.2% (4 out of 18) of patients who experienced postoperative stroke had a history of previous strokes. These findings underscore the necessity for more thorough preoperative screening.
In our study, DM was significantly associated with postoperative stroke, a relationship that has also been reported by several investigators. This further emphasizes the significance of this association that places patients at increased risk of embolization from atherosclerotic lesions as well as impaired auto-regulation of cerebral blood flow. [ 10 , 17 , 18 , 19 ]
In our sample, it was observed that over half of the stroke patients had a history of hypertension. This observation raises the possibility of an association between hypertension and stroke, consistent with the findings of some previous reports. [ 10 ] However, our analysis did not yield a statistically significant result, which may be attributed to the limited sample size.
Severe perioperative hemodilutional anemia may be a critical factor in the pathogenesis of postoperative ischemia and stroke. In our study, perioperative anemia was a risk factor of postoperative stroke. This was reported by Kulier et al. [ 26 ]. However, different other studies didn’t confirm this finding [ 27 , 28 ].
In our study, we revealed that patients with MVAC were at 3.6 times greater risk compared to those without. Several studies have highlighted that MVAC introduces considerable technical complexity to procedures involving the mitral valve, increased risk of embolization, and potentially leads to increased risks not only in operative mortality but also in perivalvular leak and atrioventricular groove disruption [ 20 , 21 , 22 ]. It is worth noting that Kaneko et al. [ 25 ] in their retrospective study of 197,737 unique MV procedures conducted at 1158 participating institutions, did not achieve statistically significant results in this context. This underscores the critical need for additional research in this area.
In our study, patients with CPB time longer than two hours and aortic cross-clamp longer than one and a half hours were associated with postoperative stroke. These prolonged times usually indicate operating on complicated combined procedures or due to unexpected unfavorable anatomy and intraoperative complications. This association has been reported by other investigators. [ 10 ]
Stroke poses a significant challenge following surgical valve replacement (SVR), affecting approximately 5% of patients. The incidence of stroke can vary based on surgical factors. From our single-center database analysis, several independent risk factors for perioperative stroke were identified. Understanding these factors is crucial for devising strategies to mitigate stroke risk through rigorous pre-, intra-, and post-operative protocols.
It is important to acknowledge the retrospective nature of this analysis, which inherently carries limitations such as potential biases in data collection. The study’s retrospective design and the relatively low number of stroke cases may limit the generalizability of our findings. Furthermore, the etiology of strokes (embolic, thrombotic, or hypoperfusive) could not be definitively determined from our data.
Limitations
Our study highlights age, atrial fibrillation (AF), prior stroke history, and double valve surgery (AVR + MVR) as significant factors associated with postoperative stroke, which are known confounders. Despite these biases, our study provides new insights into stroke risk following surgical valve replacement, emphasizing the need for targeted preventive strategies.
Additionally, the study did not systematically track patients who underwent left atrial appendage occlusion (LAAO), limiting our ability to assess its impact on stroke outcomes.
Another limitation is the low incidence of postoperative strokes, with only 18 out of 417 patients experiencing this event over 18 years. This small sample size limits the statistical power and generalizability of our findings. However, our study still offers valuable insights into the incidence and risk factors of postoperative strokes, contributing to future research and clinical practices.
Data availability
No datasets were generated or analysed during the current study.
Messé SR, Acker MA, Kasner SE, Fanning M, Giovannetti T, Ratcliffe SJ, Bilello M, Szeto WY, Bavaria JE, Hargrove WC 3rd, Mohler ER, Floyd TF 3rd. (2014) Stroke after aortic valve surgery: results from a prospective cohort. Circulatio 129:2253-61.
Daneault B, Kirtane AJ, Kodali SK, Williams MR, Genereux P, Reiss GR, Smith CR, Moses JW, Leon MB. Stroke associated with surgical and transcatheter treatment of aortic stenosis: a comprehensive review. J Am Coll Cardiol. 2011;58:2143–50.
Article PubMed Google Scholar
Vasques F, Messori A, Lucenteforte E, Biancari F. Immediate and late outcome of patients aged 80 years and older undergoing isolated aortic valve replacement: a systematic review and meta-analysis of 48 studies. Am Heart J. 2012;163:477–85.
Filsoufi F, Rahmanian PB, Castillo JG, Bronster D, Adams DH. Incidence, imaging analysis, and early and late outcomes of stroke after cardiac valve operation. Am J Cardiol. 2008;101:1472–8.
Rice CT, Barnett S, O’Connell SP et al. (2023) Impact of gender, ethnicity and social deprivation on access to surgical or transcatheter aortic valve replacement in aortic stenosis: a retrospective database study in England. Open Heart 10.
Shahian DM, O’Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP. (2009) The Society of thoracic surgeons 2008 cardiac surgery risk models: part 3–valve plus coronary artery bypass grafting surgery. Ann Thorac Surg 88(1 suppl).
O’Brien SM, Shahian DM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP. (2009) The Society of thoracic surgeons 2008 cardiac surgery risk models: part 2–isolated valve surgery. Ann Thorac Surg 88(1 suppl).
Fanning JP, Campbell BCV, Bulbulia R, et al. Perioperative stroke. Nat Rev Dis Primers. 2024;10:3.
Santos DPAD, Thirumala PD, Reddy G, Barros DF, Faria VNR, Shandal V, Kurtz P. Risk of perioperative stroke and cerebral autoregulation monitoring: a systematic review. Arq Neuropsiquiatr. 2022;80(12):1196–203.
Article PubMed PubMed Central Google Scholar
Bucerius J, Gummert JF, Borger MA, et al. Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg. 2003;75:472–8.
Baker RA, Hallsworth LJ, Knight JL. Stroke after coronary artery bypass grafting. Ann Thorac Surg. 2005;80:1746–50.
Browne A, Spence J, Power P, Copland I, Mian R, Gagnon S, Kennedy S, Sharma M, Lamy A. Perioperative covert stroke in patients undergoing coronary artery bypass graft surgery. JTCVS Open. 2020;4:1–11.
Floyd TF, Shah PN, Price CC, et al. Clinically silent cerebral ischemic events after cardiac surgery: their incidence, regional vascular occurrence, and procedural dependence. Ann Thorac Surg. 2006;81:2160–6.
Almassi GH, Sommers T, Moritz TE, Shroyer AL, London MJ, Henderson WG, Sethi GK, Grover FL, Hammermeister KE. Stroke in cardiac surgical patients: determinants and outcome. Ann Thorac Surg. 1999;68(2):391–7.
Article PubMed CAS Google Scholar
Russo A, Grigioni F, Avierinos JF, Freeman WK, Suri R, Michelena H, et al. Thromboembolic complications after surgical correction of mitral regurgitation: incidence, predictors, and clinical implications. J Am Coll Cardiol. 2008;51:1203–11.
Mavridis T, Choratta T, Papadopoulou A, Sawafta A, Archontakis-Barakakis P, Laou E, Sakellakis M, Chalkias A. Protease-activated receptors (PARs): Biology and therapeutic potential in Perioperative Stroke. Transl Stroke Res; 2024.
Arslanoğlu E, Kara KA, Yiğit F, Arkan C, Uslu U, Şavluk ÖF, Yılmaz AA, Tunçer E, Çine N, Ceyran H. Neurological complications after pediatric cardiac surgery. Cardiothorac Surg. 2021;29(1):19.
Feilberg Rasmussen L, Andreasen JJ, Riahi S, Lundbye-Christensen S, Johnsen SP, Andersen G, Mortensen JK. (2022) Risk and subtypes of stroke following new-onset postoperative atrial fibrillation in coronary bypass surgery: a population-based cohort study. J Am Heart Assoc 11(24).
Wagner BD, Grunwald GK, Hossein Almassi G, Li X, Grover FL, Shroyer ALW. Factors associated with long-term survival in patients with stroke after coronary artery bypass grafting. J Int Med Res. 2020;48(7):300060520920428.
Bedeir K, Kaneko T, Aranki S. Current and evolving strategies in the management of severe mitral annular calcification. J Thorac Cardiovasc Surg. 2018;157:555–66.
Nakai T, Okada Y, Adachi K, Muro T. Surgical treatment for degenerative mitral stenosis associated with aortic valve stenosis: a case report. J Cardiol Cases. 2023;29(3):120–3.
Ascione G, Denti P. Mitral annular calcification in patients with significant mitral valve disease: an old problem with new solutions. Front Cardiovasc Med. 2022;9:1033565.
Raffa G, Agnello F, Occhipinti G, et al. Neurological complications after cardiac surgery: a retrospective case-control study of risk factors and outcome. J Cardiothorac Surg. 2019;14:23.
Selim M. (2007) Perioperative stroke. N Engl J Med 356(7):706–713. https://doi.org/10.1056/NEJMra062668 . PMID: 17301301.
Kaneko T, Hirji S, Percy E, Aranki S, McGurk S, Body S, Heydarpour M, Mallidi H, Singh S, Pelletier M, Rawn J, Shekar P. Characterizing risks associated with mitral annular calcification in mitral valve replacement. Ann Thorac Surg. 2019;108(6):1761–7.
Kulier A, Levin J, Moser R, Rumpold-Seitlinger G, Tudor IC, Snyder-Ramos SA, Moehnle P, Mangano DT. Impact of preoperative anemia on outcome in patients undergoing coronary artery bypass graft surgery. Circulation. 2007;116:471–9.
Bahrainwala ZS, Grega MA, Hogue CW, Baumgartner WA, Selnes OA, McKhann GM, Gottesman RF. Intraoperative hemoglobin levels and transfusion independently predict stroke after cardiac operations. Ann Thorac Surg. 2011;91:1113–8.
Boening A, Boedeker RH, Scheibelhut C, Rietzschel J, Roth P, Schönburg M. Anemia before coronary artery bypass surgery as additional risk factor increases the perioperative risk. Ann Thorac Surg. 2011;92:805–10.
Download references
Acknowledgements
We received no funding for this study.
Author information
Authors and affiliations.
Faculty of Medicine, Faculty of medicine, Jordan University of Science and Technology, Irbid, Jordan
Nizar Alwaqfi, Majd M. AlBarakat, Hala Qariouti, Khalid Ibrahim & Nabil alzoubi
You can also search for this author in PubMed Google Scholar
Contributions
M.M.A and N.A validated the idea. H.Q collected the data. M.M.A. analyzed the data and wrote the manuscript. N.A, K.I, and N.A did the supervision and reviewing of the manuscript.
Corresponding author
Correspondence to Nizar Alwaqfi .
Ethics declarations
Conflict of interest.
The authors declare no conflict of interest.
Ethics approval and consent to participate
The Institutional Review Board (IRB) of Jordan University of Science and Technology approved the study with the number 519 of the year 2023. Consent forms were obtained from the patients before participation and the study followed the World Health Organization Declaration on the Ethical Principles of Helsinki for Medical Research on Humans.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Alwaqfi, N., AlBarakat, M.M., Qariouti, H. et al. Stroke after heart valve surgery: a single center institution report. J Cardiothorac Surg 19 , 518 (2024). https://doi.org/10.1186/s13019-024-03009-x
Download citation
Received : 01 January 2024
Accepted : 13 August 2024
Published : 09 September 2024
DOI : https://doi.org/10.1186/s13019-024-03009-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Heart valve surgery
- Valve surgery complications

Journal of Cardiothoracic Surgery
ISSN: 1749-8090
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
High-intensity cycling exercise after a stroke: a single case study
Affiliation.
- 1 Rivermead Rehabilitation Centre, Oxford, UK.
- PMID: 11128730
- DOI: 10.1191/0269215500cr363oa
Aerobic exercise training has demonstrated positive effects after brain injury. However, therapists express concern regarding the use of effortful exercise in individuals presenting with spasticity or involuntary muscle activity. This study aimed to address this concern and to evaluate whether an intervention of maximal intensity cycling exercise impaired an individual's ability to actively extend his hemiparetic elbow. Using a single case design, it was shown that active elbow extension improved during the period of this investigation, and was not impaired immediately following maximal cycling exercise.
PubMed Disclaimer
Similar articles
- The role and effects of rehabilitation exercise therapy for poststroke hemiparetic muscle spasticity. Zeng Z, Zhang S, DU Y, Lv Z. Zeng Z, et al. Minerva Med. 2024 Apr;115(2):230-233. doi: 10.23736/S0026-4806.23.08953-X. Epub 2023 Dec 12. Minerva Med. 2024. PMID: 38088057 No abstract available.
- Transcutaneous electrical nerve stimulation combined with task-related training improves lower limb functions in subjects with chronic stroke. Ng SS, Hui-Chan CW. Ng SS, et al. Stroke. 2007 Nov;38(11):2953-9. doi: 10.1161/STROKEAHA.107.490318. Epub 2007 Sep 27. Stroke. 2007. PMID: 17901383 Clinical Trial.
- Assisted movement with enhanced sensation (AMES): coupling motor and sensory to remediate motor deficits in chronic stroke patients. Cordo P, Lutsep H, Cordo L, Wright WG, Cacciatore T, Skoss R. Cordo P, et al. Neurorehabil Neural Repair. 2009 Jan;23(1):67-77. doi: 10.1177/1545968308317437. Epub 2008 Jul 21. Neurorehabil Neural Repair. 2009. PMID: 18645190 Clinical Trial.
- Clinical relevance of the effects of reach-to-grasp training using trunk restraint in individuals with hemiparesis poststroke: A systematic review. Greisberger A, Aviv H, Garbade SF, Diermayr G. Greisberger A, et al. J Rehabil Med. 2016 Apr 28;48(5):405-16. doi: 10.2340/16501977-2077. J Rehabil Med. 2016. PMID: 27008369 Review.
- Benefits of aerobic exercise after stroke. Potempa K, Braun LT, Tinknell T, Popovich J. Potempa K, et al. Sports Med. 1996 May;21(5):337-46. doi: 10.2165/00007256-199621050-00003. Sports Med. 1996. PMID: 8724202 Review.
- The effect of involuntary motor activity on myoelectric pattern recognition: a case study with chronic stroke patients. Zhang X, Li Y, Chen X, Li G, Rymer WZ, Zhou P. Zhang X, et al. J Neural Eng. 2013 Aug;10(4):046015. doi: 10.1088/1741-2560/10/4/046015. Epub 2013 Jul 17. J Neural Eng. 2013. PMID: 23860192 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
The Values-Based Culture and Legacy of Brights Hardware: A Single Case Study
- First Online: 11 September 2024
Cite this chapter

- Karen Cerff 8
Part of the book series: Christian Faith Perspectives in Leadership and Business ((CFPLB))
This case study focused on Brights Hardware, which was established in South Africa in 1971. The original supermarket store carried a few hardware items. In 2021, Brights Hardware celebrated its 50th birthday, having expanded to over 900 employees at 9 retail branches and an online store providing national coverage. The family-owned group includes family members from three generations who work for the organization. The initial values which the founders embraced and advanced have been challenged and refined over the years. These values are continuously demonstrated and communicated across the generations of the family and to the employees within the unique organizational culture. This case study explored the history and transitions from a small business to multiple sites, becoming an organization of significance in its niche, and known for its values-driven leadership. Brights has led the way in the industry nationally in applying new strategies, and in withdrawing from popular business practices to promote family values. Brights has achieved a strong reputation as a professional and friendly family business where employees are regarded as a form of family, where high levels of ethics, loyalty, a fair returns policy and innovation characterize the organization and contribute to the ongoing growth and success.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Bass, B. M. (1990). Bass & Stogdill’s handbook of leadership: Theory, research, & managerial applications (3rd ed.). Free Press.
Google Scholar
Bommer, M., Gratto, C., Gravander, J., & Tuttle, M. (1987). A behavioral model of ethical and unethical decision making. Journal of Business Ethics, 6 , 265–280.
Article Google Scholar
Brights Hardware Store. (2022). About . https://www.brights.co.za/about-brights-hardware/
Brights Strategic Plan 2023 . Unpublished document.
Carabi, A. (2017). Organizational tribes: A tribal approach to well-being and belonging for business . Medium. https://alexcarabi.medium.com/organizational-tribes-c8f762ca014
Cerff, K. (2008). Towards establishing and promoting ethical standards in organizations in South Africa: A single-case study . Paper presented at the Christian Leadership Colloquium with St. Augustine College, Johannesburg.
CFA Properties. (2023). Who we are . https://www.chick-fil-a.com/about/who-we-are
Colson, C., & Pearcey, N. (1999). How now shall we live? Tyndale House.
Daft, R. L. (2005). The leadership experience (3rd ed.). South-Western.
Encyclopaedia Britannica . (2024). Mozambique under the New State regime . https://www.britannica.com/place/Mozambique/Mozambique-under-the-New-State-regime
Fritzsche, D. J. (1991). A model of decision-making incorporating ethical values. Journal of Business Ethics, 10 , 841–852.
Global Voice of Prayer. (N.d.). https://www.globalvoiceofprayer.com/
Green, D., & High, B. (2017). Giving it all away… and getting it all back again: The way of living generously . HarperCollins.
Hobby Lobby. (2024). https://www.hobbylobby.com/
Ismael, J. S. (2001). South Africa’s Sunday laws: Finding a compromise. Indiana Comparative and International Law Review, 12 (1), 563–585.
Luis, M. (2023). When all is said and done. Unpublished manuscript.
New King James Version. (1982). https://www.biblegateway.com/versions/New-King-James-Version-NKJV-Bible/
Pascarella, P. (1999). Christ-centered leadership: Thriving in business by putting God in charge . Prima.
Power Group. (N.d.). https://www.powergrp.co.za/
Quintal, G. (2012, March 13). Public protector: What we need are ethical leaders. Mail & Guardian . https://mg.co.za/article/2012-03-13-what-we-need-are-ethical-leaders-public-protector/
Sauser, W. I. (2005). Ethics in business: Answering the call. Journal of Business Ethics, 58 (4), 345–357.
Schein, E. H. (2004). Organizational culture and leadership (3rd ed.). Jossey-Bass.
Strong, K. C., & Meyer, G. D. (1992). An integrative descriptive model of ethical decision making. Journal of Business Ethics, 11 , 89–94.
Sutter, B. (2023). How hard small business owners work . Score. https://www.score.org/resource/blog-post/how-hard-small-business-owners-work
Unashamedly Ethical. (2021). https://unashamedlyethical.com/about-us/
Webster, N. (1967). American dictionary of the English language: Noah Webster 1828 . The Foundation of American Christian Education.
Wessels, C. (2022, March 22). Why family businesses fail. Moneyweb. https://www.moneyweb.co.za/financial-advisor-views/why-family-businesses-fail/#:~:text=Risks%20in%20a%20family%20business&text=Structures%20with%20regards%20to%20shareholding,in%20the%20business%20become%20more
World Justice Project. (N.d.). Thuli Madonsela . https://worldjusticeproject.org/world-justice-forum-vi/thuli-madonsela/
Yin, R. K. (1994). Case study research: Design and methods (2nd ed.). Sage.
Yukl, G. (2002). Leadership in organizations (5th ed.). Prentice Hall.
Download references
Author information
Authors and affiliations.
Transformational Leadership Institute, Johannesburg, South Africa
Karen Cerff
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Karen Cerff .
Editor information
Editors and affiliations.
School of Business & Leadership, Regent University, Virginia Beach, VA, USA
John Mulford
Emilyn Cabanda
Andrew Root
Department of Business, Pfeiffer University, Misenheimer, NC, USA
Raushan Gross
Rights and permissions
Reprints and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cerff, K. (2024). The Values-Based Culture and Legacy of Brights Hardware: A Single Case Study. In: Mulford, J., Cabanda, E., Root, A., Gross, R. (eds) Faith-Based Entrepreneurship. Christian Faith Perspectives in Leadership and Business. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-031-65199-1_9
Download citation
DOI : https://doi.org/10.1007/978-3-031-65199-1_9
Published : 11 September 2024
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-031-65198-4
Online ISBN : 978-3-031-65199-1
eBook Packages : Business and Management Business and Management (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Experimental study on single-cylinder two-stroke piston expander based on in-cylinder spray heat transfer
Compressed air energy storage stands as a highly promising technology within the realm of energy retention. The piston expander finds applicability in smaller-scale compressed air energy storage systems. In compressed air energy storage systems, the expansion process is critical in energy discharge and significantly impacts overall performance. Isothermal expansion techniques are effective in enhancing the operational efficiency of piston expanders, in contrast to adiabatic expansion methodologies. Previous simulations by our research group show that the isothermal expansion model has a lower power output than the adiabatic expansion model due to its higher exhaust pressure. To further validate the accuracy of the simulation results, an experimental platform was constructed and the uncertainty of the experimental system as well as the measured data was evaluated. This study conducted experimental research using the single-variable method, focusing on different load conditions and spray parameters. The study findings indicate that the exhaust pressure during isothermal expansion consistently exceeds that of adiabatic expansion. The exhaust pressure of isothermal expansion increased by 3.85 % to 14.9 %. Under varying load conditions, the average rotational speed and output power of isothermal expansion were noted to be inferior to those of adiabatic expansion. Despite changes in nozzle diameter or spray temperature when the spray timing is set at 0°-180°, the average rotational speed and output power of isothermal expansion remain lower than that of adiabatic expansion. The average output power of isothermal expansion decreased by 1.29 % to 5.24 %. Nevertheless, if the spray timing is set between 0°-120°, the average output power of the isothermal expansion surpasses the adiabatic expansion with an improvement of 1.84 %.
1. Introduction
In the persistent promotion of the “double carbon” strategy, China's installed capacity for renewable energy has demonstrated substantial annual growth. According to the renewable energy installed capacity data released by the National Energy Administration (NEA) [1], the newly installed capacity in 2022 reached 1.52×10 8 kW, constituting 76.2 % of the recently added power generation capacity. This has evolved into China's predominant component of newly installed power capacity.
The inherent intermittency and uncertainty of renewable energy pose challenges to grid-connected consumption, impeding the attainment of an economically balanced power supply and demand [2, 3]. Consequently, there arises a pressing necessity for one or more electric energy storage technologies to address the complexities inherent in the processes of renewable energy electricity production, storage, and consumption. In contrast to alternative energy storage technologies, compressed air energy storage (CAES) boasts distinct advantages encompassing an extended lifespan, environmentally benign characteristics, robust safety and reliability, and expansive application potential. The inaugural commercially operational CAES power plant, Huntorf in Germany, marked a pioneering achievement. Presently, the system achieves an output power of 321MW. An additional milestone in the realm of CAES is the inaugural megawatt-level isothermal system, realized by the American company SustainX, demonstrating a commendable operational longevity of up to two decades [4].
The compressor/expander is a pivotal element of the CAES system, and with the premise of dealing with the thermal aspects of compression/expansion [5], CAES technology is demarcated into diabatic CAES (D-CAES), adiabatic CAES (A-CAES without Thermal Energy Storage (TES), A-CAES with TES) and isothermal CAES (I-CAES). In the ideal I-CAES cycle, using the isothermal compress/expand process can reduce compressing power and increase expanding power compared to the adiabatic process [6, 7]. Attaining isothermal compression/expansion of gases through conventional mechanical apparatus has, until now, posed a formidable challenge [8]. The majority of mechanical devices find themselves situated between adiabatic compression/expansion and isothermal compression/expansion, occupying a realm often described as near-isothermal compression/expansion [9]. The primary obstacle in realizing near-isothermal compression/expansion lies in effectively facilitating swift heat transfer during air compression/expansion. Current technologies addressing rapid heat transfer predominantly involve liquid piston heat transfer [10] and water spray heat transfer.
The piston expander exhibits characteristics of low speed and high torque. Research indicates the piston expander's superior suitability for small CAES systems [11, 12]. Nevertheless, challenges arise from the inefficiency of the conventional adiabatic expansion model (AEM), leading to suboptimal expander efficiency and susceptibility to freezing and clogging at the exhaust port, hindering widespread application in CAES systems. Presently, there is a notable scholarly focus on enhancing expander output performance through the application of the aforementioned heat transfer technology.
In terms of heat transfer of liquid pistons, Andrew et al. [13] optimized the power and efficiency based on the air compression and expansion process of liquid piston, and obtained the optimal value of heat transfer coefficient and heat transfer area under the specified volume. Due to the limited heat transfer area of the liquid piston, many scholars have introduced porous media and water spray heat transfer into the liquid piston I-CAES system to increase the heat transfer area, so that compression/expansion is closer to the isothermal process. Jacob et al. [14] investigated experimentally the effect of the introduction of porous media on the efficiency and power density of a liquid piston gas compression/expansion machine under high-pressure conditions and showed that the efficiency reached 93 %. Under the same conditions, the compression and expansion working power densities were 10 and 20 times higher than the power density without the introduction of porous media, respectively. Chen et al. [15] achieved efficient continuous near-isothermal compression energy storage and expansion energy release of air by using two pressure vessels with liquid pistons and intensifying the isothermal compression/expansion process by spraying water mist into the two pressure vessels, and the indicated and round-trip efficiencies of the system were obtained as high as 98 % and 76 %, respectively, and the temperature rise during air compression and temperature drop during air expansion were within 5 °C. Zhao et al. [16] also make use of the similar pressure vessel mentioned above, but discard the gas storage device in the compressed air energy storage system. After one isothermal compression/expansion of each pressure vessel, the system completes one cycle, achieving a stable output power of the system. The research results show that the round-trip efficiency of the system is 61.42 %, and the energy density is 0.2015 kWh/m 3 . Although the liquid piston improves the efficiency of heat exchange in the expansion process, the gas brought into the hydraulic system will cause a reduction in the elastic modulus of the liquid, increased noise and vibration, increased wear, and cavitation in the low-pressure region, affecting its further application. The coupling of liquid pistons with various heat transfer methods leads to complex system structures and high production costs.
In terms of heat transfer of water spray, SustainX (USA) has compared experimental data of AEM and isothermal expansion model (IEM) in its 2015 technical report [17]. Under the same air quality, the gas temperature after expansion of without water mist gas is 175 °C lower than the initial ambient temperature, and the adiabatic efficiency is 54 %. The difference between the gas temperature after expansion with water mist and the initial ambient temperature is 15 °C, the isothermal efficiency is 95 %, and the output time of the same constant power is 65 % longer than the expansion time without water mist. The above experiment requires a slower expansion stroke. Zhang et al. [18] conducted an experimental test on a single-valve reciprocating expander and verified the correctness of the AEM. Then, the water mist-air heat transfer equation was introduced to achieve near-IEM of gas. The simulation results show that the temperature difference of near-IEM is only 10% of that of AEM, and the specific energy increases by 15.7 %. However, the near-isothermal model has not been verified by experiments. Braasch et al. [19] built an experimental device that could measure the parameters of the gas expansion process, and the experimental test showed that near-IEM of gas could be achieved by spraying water mist into the atmosphere with nitrogen or helium gas. The results show that the output work of the isothermal process can reach 94.2 %. Although Braasch al. proved the effectiveness of near-IEM of gas by using water mist heat transfer through experiments, they did not apply it to a real expander to analyze the whole process. Our research group [20] has simulated the single-cylinder two-stroke piston expander (SCTS-PE) based on spray heat transfer in the early stage and found that the injection of high-temperature water mist during the expansion of compressed air can effectively restrain the air temperature drop and increase the air pressure in the cylinder. As the heat transfer through water mist leads to the increase of gas pressure in the exhaust process, the output power and efficiency are reduced.
Based on the previous research conducted by our research group, this study aims to further validate the accuracy of the simulations by investigating the performance of a single-cylinder, SCTS-PE based on in-cylinder spray heat transfer through experimental research. The main focus is on studying the effects of three parameters: nozzle diameter, spray temperature, and spray timing on the expander. This is also the first time that IEM has been applied to the entire working process of a SCTS-PE.
The rest of this paper is organized as follows: Section 2 provides a detailed explanation of the working principles of the SCTS-PE and its ideal isothermal/adiabatic thermodynamic cycle. Section 3 describes in detail the experimental equipment and experimental procedures of the experimental bench, as well as the uncertainty assessment of the measured parameters. Section 4 is about the results and discussion of the experiment. Finally, Section 5 provides a summary of the experimental findings.
2. Description of the SCTS-PE and the ideal IEM/AEM thermodynamic cycle
2.1. working principle of scts-pe.
This study selected the third-generation SCTS-PE prototype developed by our research group and the prototype of this SCTS-PE and its section diagram of valve timing mechanism [21] are shown in Fig. 1. As with conventional internal combustion engines, a mechanically driven valve timing mechanism is used to control the gas flow during the intake and exhaust processes. The valve timing mechanism is composed of valve combination (valve, valve seat, valve guide, valve spring) and valve transmission group (camshaft, camshaft transmission mechanism). The working process of SCTS-PE can be divided into the intake process, expansion process, and exhaust process. The motion cycle is shown schematically in Fig. 2. The kinematic scheme and detailed mathematical modeling of this SCTS-PE have been published in the literature [20]. The cam lift curve of the valve timing mechanism should be rectangular in ideal condition, that is, the maximum lift can be reached when the valve is opened, and the maximum lift is always maintained within the intake duration angle, but it is closed immediately when it is closed so that the throttling loss of the expander will be reduced. The optimal maximum lift of intake and exhaust valves and the optimal gas distribution phase have been obtained in the simulation optimisation process [22]. In the actual operation of the piston expander, the time of a single gas distribution cycle will change depending on the rotational speed, but the gas distribution phase and the maximum lift of the valves will not change. Due to the good followability of the cam-based gas distribution system, we considered the cam lift during its operation to be the same as that obtained from the simulation optimisation. The intake and exhaust valve lift curves obtained from the simulation optimisation are shown in Fig. 3.
Fig. 1 The prototype of SCTS-PE and its section diagram of the valve timing mechanism
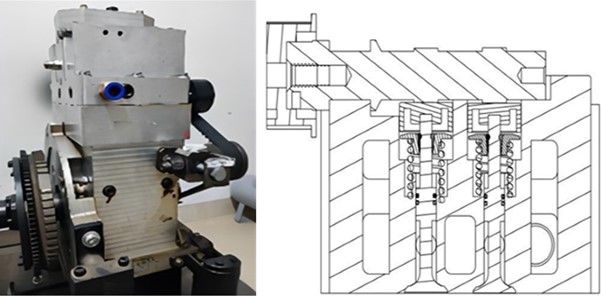
Fig. 2 Schematic diagram of SCTS-PE work cycle
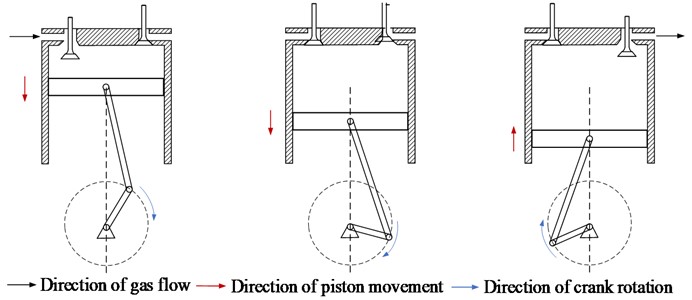
Fig. 3 Lift curve of intake and exhaust valves
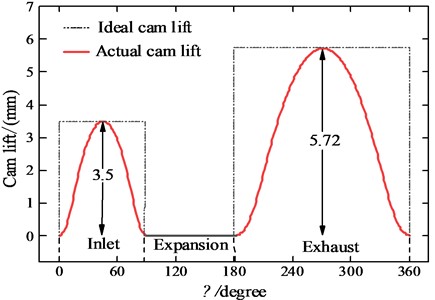
2.2. Thermodynamic cycle of IEM/AEM
When the valve structure is in the form of an ideal opening and closing (ideal CAM lift shown in Fig. 3), the thermodynamic cycle of the SCTS-PE is shown in Fig. 4. The ideal IEM/AEM thermodynamic cycle of the SCTS-PE consists of an equal mass isentropic/isothermal process: 3-4, 3-4′; two variable-mass isentropic processes: 1-2 and 4-5; and two variable-mass isobaric processes: 2-3 and 5-1.
Fig. 4 The p-V diagram of ideal IEM/AEM
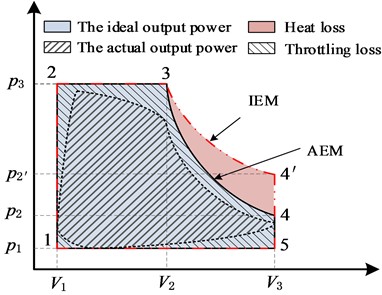
In stages 1-2, the intake valve is opened, compressed air enters the cylinder and quickly fills the cylinder clearance V 1 , making the gas pressure in the cylinder rise rapidly to p 3 . At this time, the piston is stationary at the top dead center (TDC) and the gas does not work on the piston. In the actual process (actual lift curve of intake and exhaust valves shown in Fig. 3), due to the intake valve not directly reaching the maximum lift, the pressure in the cylinder clearance should be lower than p 3 .
In stages 2-3, compressed air flows continuously into the cylinder to keep the pressure in the cylinder constant and the piston moves from TDC to bottom dead center (BDC). When the cylinder content volume changes from V 1 to V 2 , the intake valve closes quickly, and the external work done at this stage can be expressed by Eq. (1). Of course, in the actual process, certain throttle loss will be caused when the intake valve is opened and closed. The pressure in the cylinder at stages 2-3 is not constant and the pressure of the gas in the cylinder is less than p 3 :
In stages 3-4/ 3-4′, the intake valve and exhaust valve are closed, and the gas in the cylinder with a constant mass pushes the piston to do work. If the gas does not exchange heat with the outside world, it is an ideal AEM, such as stages 3-4 in the figure, whose external output work can be expressed by Eq. (2), where k is the gas adiabatic index. If the temperature of the gas is constant in the expansion process, that is, IEM, the pressure of the gas in the cylinder will decrease at a slower rate and improve the mechanical work output. As shown in Fig. 4, stages 3-4′, the external output mechanical work of IEM can be expressed by Eq. (3). Ideal AEM results in heat loss compared to IEM. AEM results in an increase in the volume of the gas and a decrease in the pressure during expansion due to the lack of heat exchange with the outside world during expansion, which also results in a decrease in temperature. In IEM, the gas inside the cylinder can exchange heat and the temperature inside the cylinder remains constant. In realistic SCTS-PE in the gas expansion process, the gas is difficult to achieve absolute isothermal/adiabatic expansion, the pressure curve is lower than the IEM pressure curve is higher than the AEM pressure curve:
In stages 4-5/ 4-5′, when the piston reaches BDC and the exhaust valve opens, the fluid from the cylinder is discharged when the piston is fixed at BDC, resulting in a rapid drop in cylinder pressure and no work done by the gas on the piston. In the actual process, this stage is analogous to the 1-2 stage, the air pressure in the cylinder of this process is much larger than p 1 .
In stages 5-1, the compressed gas within the cylinder is discharged out of the cylinder, but at this time the gas temperature and pressure are reduced, and the energy contained in it is correspondingly reduced, the role of the outside world can be expressed in Eq. (4). Of course, in the actual process, when the exhaust valve is closed, certain throttling loss will be caused. The pressure in the cylinder at the 5-1 stage is also not a constant and the pressure of the gas in the cylinder is greater than p 1 , and the hindering force of the real gas on the piston is greater:
The AEM output work ( W a ) and IEM output work ( W i ) of SCTS-PE under one operating cycle can be expressed by the Eq. (5):
The above is the adiabatic/isothermal output work of the ideal valve lift. The area included in the p - V of the actual SCTS-PE is within the area included in the adiabatic/isothermal p - V , the actual output power is shown in Fig. 4.
3. Experiments
3.1. description of the test bench.
Fig. 5 shows the schematic diagram of the IEM system test platform, which is mainly composed of an air expansion system, a high-pressure water mist system, and a data acquisition system.
Air expansion system: The atmosphere is compressed, filtered, and separated by the air compressor and stored in the gas tank. The high-pressure air in the gas tank is decompressed by the manual pressure-reducing valve and then enters the SCTS-PE to push the piston to do work. During operation, the magnetic powder brake provides a stable load for the SCTS-PE.
Fig. 5 The schematic diagram of the system test platform: 1 – constant temperature box; 2 – water mist generator; 3 – high-frequency solenoid valve; 4 – data processing computer; 5 – Data acquisition system; 6 – exhaust valve stem; 7 – high-pressure nozzle head; 8 – micro dynamic pressure transmitter; 9 – intake valve stem; 10 – manual pressure-reducing valve; 11 – air storage tank; 12 – air compressor; 13 – serial port converter; 14 – hall sensor; 15 – piston head; 16 – magnetic powder brake; 17 – coupling; 18 – torque sensor; 19 – coupling; 20 – signal flywheel; 21 – crankshaft; 22 – exhaust channel; 23 – nozzle channel; 24 – pressure sensor channel; 25 – intake channel, A-A cylinder head cross-sectional view
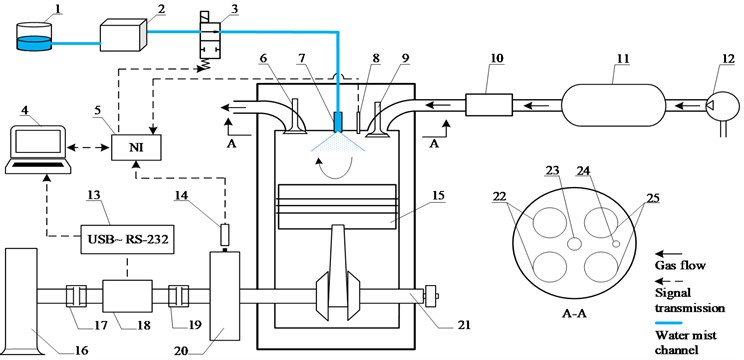
High-pressure water mist system: The opening and closing of the high-frequency ringing solenoid valve are controlled by the crankshaft phase angle signal collected by the Hall sensor. When the high-frequency solenoid valve is in the open state, the high-temperature water flow of the constant temperature tank is pressurized by the water mist generator and flows into the nozzle to atomize the water. The atomized water flow contacts with the gas in the cylinder for heat transfer.
Data acquisition system: The torque sensor mounted on the crankshaft collects the speed, torque, and power data during operation, and the data is collected on the computer through a serial converter. The miniature dynamic pressure transmitter is used to collect the air pressure in the cylinder and output the analog quantity to the NI data acquisition card. The data is displayed and stored in real time by LabVIEW.
Table 1 Main components selection summary
The test bench is shown in Fig. 6, and the selection of main components is summarized in Table 1. The cylinder diameter of the single-cylinder two-stroke PE is 0.085 m, the cylinder stroke is 0.088m, and the cylinder clearance is 3.97×10 -5 m. The cylinder head of the expander is equipped with a nozzle head and a miniature dynamic pressure transmitter, and the cylinder head is shown in Fig. 7. The droplet diameter can be adjusted by changing different nozzle models. The micro-dynamic pressure transmitter can measure conventional gas/liquid to meet the needs of the working conditions.
Fig. 6 Physical picture of the test system: 1 – air inlet; 2 – SCTS-PE; 3 – miniature dynamic pressure transmitter; 4 – hall sensor; 5 – high-frequency solenoid valve; 6 – torque sensor; 7 – magnetic powder brake; 8 – NI acquisition card; 9 – transformer; 10 – torsion, speed, and power display instrument; 11 – magnetic powder brake controller; 12 – data processing computer; 13 – water mist generator; 14 – constant temperature box; 15 – manual pressure-reducing valve; 16 – air compressor and air storage tank
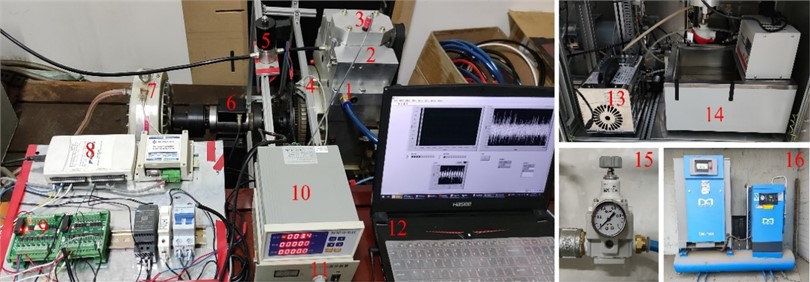
Fig. 7 Installation design drawing of high-pressure nozzle head: 1 – air inlet; 2 – intake valve; 3 – measurement cylinder pressure hole; 4 – exhaust valve; 5 – exhaust port; 6 – installation nozzle design hole 7 – high-pressure nozzle head 8 – miniature dynamic pressure transmitte
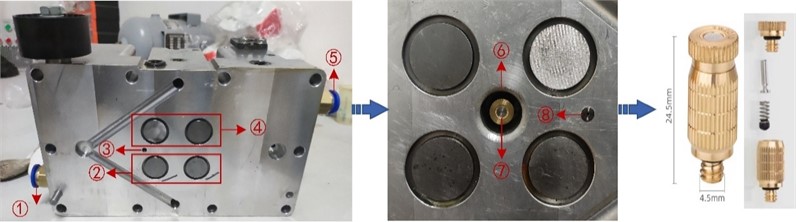
The injection of water mist in the exhaust process will increase gas pressure in the cylinder and affect the output performance of the SCTS-PE, so it is necessary to control the injection time of water mist. Since the SCTS-PE outputs rotary motion during operation, each position of the flywheel signal plate edge corresponds to a crankshaft angle. Therefore, the signal of the crankshaft angle is collected to control the high-pressure water mist system. The induction magnet and unlocking magnet are pasted at different crankshaft angles. When the flywheel rotates rapidly, the induction magnet first moves to the lower part of the induction terminal of the hall sensor to generate electricity. After sustained power generation, the unlocking magnet loses power, forming the cyclic signal acquisition of the hall sensor, and the installation position diagram of the hall sensor is shown in Fig. 8. The 5 V electrical signal collected by the hall sensor is transferred to the NI acquisition card. LabVIEW control program is used to control the output signal of the solenoid valve controlled by the NI acquisition card. The solenoid valve with a frequency response of 120 Hz is switched on and off by the transformer as a DC 24 signal, to control the duration of water spray injection into the cylinder.
4. Experimental process
Preceding the experiment, the thermostatic chamber undergoes heating to attain the targeted experimental temperature. Throughout the experiment, adjustments to the output current of the electromagnetic powder brake controller are made to variably modify the analog load facilitated by the electromagnetic powder brake. Control over the spray temperature is achieved by modulating the water temperature within the thermostatic chamber, while diverse spray timings are attained by manipulating the position of the induced magnet and the unlocking magnet. The alteration of the nozzle diameter is facilitated by its replacement. Subsequently, the ensuing steps delineate the particulars of each experiment:
1) Throughout each experimental trial, the intake pressure is meticulously regulated to attain a level of 0.6 MPa through the precise adjustment of the pressure relief valve.
2) Before each experiment, measurements are taken for the idle rotational speed and the rotational speed under a load of 4 N·m. The variation in speed from the initial experiment was utilized to standardize the speed difference for each set, guaranteeing uniform conditions for all experiments
3) Initially, employing a spray temperature of 94 ℃, a nozzle diameter of 0.15 mm, and a spray timing spanning from 0° to 180°, the investigation focused on assessing the impact of diverse loads on the AOP of the SCTS-PE by systematically varying the applied load.
4) Subsequently, employing a load of 6 N·m, a spray temperature of 94 ℃, and a spray timing spanning from 0° to 180°, the investigation delved into the ramifications of varying nozzle diameters on the SCTS-PE. Furthermore, maintaining a load of 6 N·m, a nozzle diameter of 0.15 mm, and a spray timing from 0° to 180°, the scrutiny extended to examining the influences of different spray temperatures on the SCTS-PE. Finally, under a load of 6 N·m, a spray temperature of 94 ℃, and a nozzle diameter of 0.15 mm, the exploration probed into the repercussions of altering spray timing on the SCTS-PE.
5) Throughout each experimental process, the real-time storage of pressure data and rotational speed data is executed on the computer’s E drive.
Fig. 8 Installation position diagram of hall sensor: 1 – induced magnet; 2 – unlocking magnet; 3 – hall sensor
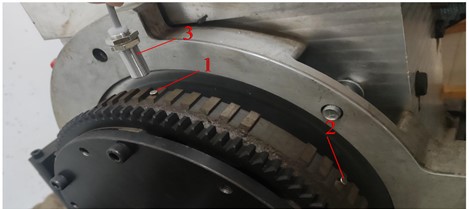
4.1. Uncertainty assessment of experimental systems
To accurately assess the reliability of the results of this experimental system, the entire experimental system is required to carry out uncertainty assessment. this section is mainly on the load torque, the in-cylinder pressure, the rotational speed and the output power to carry out the uncertainty assessment, by the literature [23] can be obtained from the uncertainty assessment in the main assessment equation. The standard uncertainty calculation equation is:
where α is the half-width of the confidence interval, k is the confidence factor, and the selection of k is related to the probability distribution and confidence level. When a measurement parameter is influenced by multiple factors, its synthetic standard uncertainty u c needs to be calculated, and the equation for u c is:
where u i is one of the standard uncertainty components and m is the number of standard uncertainty components in the system. The extended uncertainty U is calculated by the Eq. (8):
When calculating the extended uncertainty, the confidence level is taken as 95 %, and the table shows that the confidence factor is taken as k = 2.
4.2. Uncertainty analysis and calculation of cylinder pressure and load torque
After analysis, the main uncertainty components affecting the in-cylinder pressure include the uncertainty component u ∆ p of the fluctuation amplitude of the inlet pressure and the uncertainty component u p of the pressure measuring equipment, both of which belong to the uncertainty category B. The main uncertainty components affecting the load torque include the uncertainty component u p T of the equipment providing the load torque and the uncertainty component u e T of the equipment controlling the load torque, both of which also belong to the uncertainty category B.
Category B uncertainty component is mainly caused by the accuracy error of measuring equipment. In the calculation of category B uncertainty, assuming that it is a homogeneous distribution, according to the table, the confidence factor is taken as k = 3 , and according to the accuracy of the measuring equipment in Table 1, the above category B uncertainty can be calculated through Eq. (6), respectively. Through Eqs. (7-8), the synthetic standard uncertainty and extended uncertainty can be calculated respectively. The results of uncertainty calculations for cylinder pressure as well as load torque are shown in Table 2.
Table 2 Uncertainty analysis with different nozzle diameters
4.3. Uncertainty analysis and calculation of rotational speed and output power
After analysis, the main uncertainty components affecting the rotational speed include the uncertainty component u s of the rotational speed measuring equipment, which belongs to category B uncertainty, and the uncertainty component u r caused by repeated measurements, which belongs to category A uncertainty.
The calculation of category B uncertainty component u s is shown in Eq. (9):
In the calculation of category A uncertainty component u r , the sensor under the same experimental conditions, the output rotational speed of repeated measurements, each experiment on which 100 measurements are analyzed, the group of data for the average value of s - , and calculate the standard deviation S s , you can evaluate the uncertainty caused by repeated measurements under the conditions of the experiments, the calculation of the equation is as follows:
According to the power calculation Eq. (15), it can be seen that the average output power is calculated indirectly through the equation, so its uncertainty needs to be calculated through the uncertainty transfer equation, which is calculated as Eq. (16):
where n is the rotational speed and T is the load torque:
Based on the above analysis, Tables 3-5 show the mean s - , standard deviation σ , and uncertainty u c s of the rotational speed under different experimental conditions, and the uncertainty u c p of the output power was also calculated.
Table 3 Uncertainty analysis with different nozzle diameters
| (rpm) | (rpm) | |||
Table 4 Uncertainty analysis with different spray temperatures
Table 5 Uncertainty analysis with different spray timings
5. Experimental results and analysis
5.1. effect of the load on the aop of the scts-pe.
Amidst diverse loads, the operational parameters of the SCTS-PE exhibit variation, consequently influencing the output performance. To ensure the steadfast operation of the SCTS-PE at a consistent pace, loads of 2 N·m, 4 N·m, 6 N·m, 8 N·m, and 10 N·m were judiciously chosen for this experiment. In this study, the impact of IEM and AEM on the AOP of the SCTS-PE was initially explored under distinct loads. Fig. 9 shows the comparative analysis of AOP between IEM and AEM across varying loads.
Fig. 9 Comparison of AOP under different loads
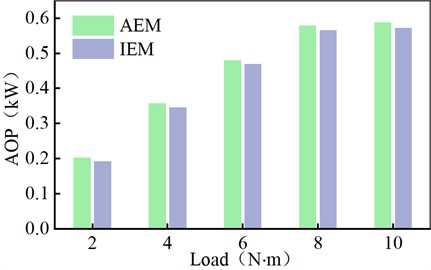
In scrutinizing the impact of diverse parameters on output power, the initial step involves ascertaining the stage of stable operation for the SCTS-PE through the collection of speed data. The procedural sequence is as follows: leveraging insights from our research group’s antecedent simulation studies, it is established that the theoretical rotational speed curve manifests sinusoidal oscillations during stable operation. Post-experiment, the gathered rotational speed data is graphically represented as a rotational speed curve, and if the difference between adjacent maximum and minimum rotational speeds falls within 10 rpm, it is deemed that the SCTS-PE has entered the stable operation phase. By calculating the average rotational speed over this period, the average output power can be calculated by Eq. (15).
The computational outcomes are visually presented in Fig. 9. In contrast to the AEM, the IEM exhibits a reduction in AOP by 2.22 %, 3.30 %, 2.08 %, 2.32 %, and 2.84 %, respectively. This discrepancy arises due to the higher gas pressure inside the IEM cylinder during the exhaust phase compared to AEM, resulting in increased resistance for the gas to perform work on the piston during exhaust. This effect outweighs that of the intake and expansion phases, thereby yielding a diminished AOP for IEM. Under a 6 N·m load, calculations unveil an ARS of 764 rpm and an AOP of 0.4797 kW for AEM, serving as foundational data for subsequent comparisons with IEM in the ensuing discussion.
5.2. Effect of nozzle diameter on the SCTS-PE
The nozzle diameter plays a pivotal role in determining the size of water mist droplets. If the droplets are excessively large, it impedes their ability to adequately exchange heat with the gas inside the cylinder upon initial entry. This, in turn, diminishes the efficiency of gas-liquid heat exchange. Conversely, reducing the droplet size augments the surface area available for contact between the liquid and gas, thereby enhancing the rate of heat transfer. Consequently, nozzle diameters are configured at 0.15 mm, 0.25 mm, and 0.35 mm, respectively. The ensuing discussion delves into the detailed impact of nozzle diameter on cylinder pressure, ARS, and AOP of the SCTS-PE.
5.3. Effect of nozzle diameter on the cylinder pressure of the SCTS-PE
The main factor affecting SCTS-PE performance is cylinder pressure. The cylinder pressure directly determines the output power of the SCTS-PE, thus influencing its overall performance. Fig. 10 shows the p - V diagram illustrating the effect of nozzle diameter on the cylinder pressure.
From Fig. 10, it can be observed that during the intake process, the cylinder gas pressure of the IEM is slightly higher than that of the AEM. This is because compressed air primarily transfers energy to drive the piston during the intake process, resulting in a smaller decrease in air temperature. As a result, the temperature difference between the water mist and the air is small, and the heat supplied by the water mist to the air is less. The cylinder gas pressure for the IEM with nozzle diameters of 0.15 mm, 0.25 mm, and 0.35 mm are relatively similar, indicating that the size of water droplets has little impact on the gas pressure during the intake process. During the expansion phase, the cylinder gas pressure for IEM is significantly higher than that of AEM. The exhaust pressure of IEM is always higher than the exhaust pressure of AEM. The exhaust pressure for AEM is 0.208 MPa. For IIEM, when the nozzle diameter is 0.15 mm, 0.25 mm, and 0.35 mm, the exhaust pressures are 0.239 MPa, 0.236 MPa, and 0.232 MPa, respectively. These values indicate an increase of 14.9 %, 13.46 %, and 11.54 % compared to AEM. This is because compressed air primarily expands to drive the piston during the intake process, and AEM leads to heat absorption by the gas, reducing the output of mechanical energy. In contrast, IEM utilizes the water mist for reheating, suppressing the temperature drop of the expanding air and allowing for more mechanical energy output. This indicates that spray heat transfer can achieve isothermal expansion of the gas, resulting in higher output pressure during the expansion phase. Smaller water droplet diameters lead to higher cylinder gas pressures during the expansion process, suggesting that smaller water droplet diameters are more favorable for heat exchange between water mist and air. During the exhaust phase, the cylinder gas pressure for IEM is also significantly higher than that of AEM. This is because although the water mist is not sprayed into the cylinder during the exhaust phase, after the heat exchange between the water mist and the air during the intake and expansion processes, the water mist still retains heat and exchanges heat with the gas during the exhaust phase.
Fig. 10 Comparison of p-V diagrams for different nozzle diameters
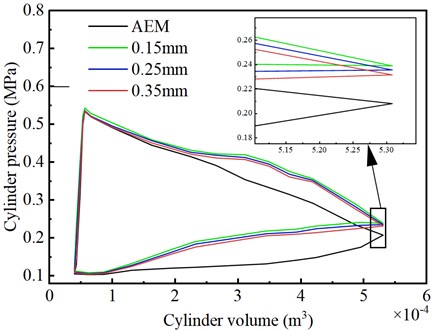
5.4. Effect of nozzle diameter on the ARS and AOP of the SCTS-PE
When studying the influence of nozzle diameter on the ARS and AOP of the SCTS-PE, the data used are from the stable operation of the SCTS-PE. Fig. 11 shows the comparison of the effects of AEM on the ARS and AOP of the SCTS-PE under different nozzle diameters.
From Fig. 11, it is possible to see that the ARS of the IEM is lower than that of the AEM. The ARS of the AEM is 764 rpm, while the ARS of the IEM are 725 rpm, 733 rpm, and 749 rpm respectively. As the nozzle diameter increases, the ARS of the IEM increases. This is mainly because a smaller nozzle diameter facilitates heat transfer between the high-temperature mist and the gas in the cylinder, resulting in higher pressure inside the cylinder. As shown in Fig. 10, the pressure inside the cylinder has a significant influence on the exhaust phase, leading to greater gas resistance to piston work during the exhaust process. Therefore, with a nozzle diameter of 0.15 mm, the ARS displays a relatively lower value.
Similarly, it is possible to observe that the AOP of the IEM with different nozzle diameters is lower than that of the AEM. The AOP of the IEM increases with the increase in the nozzle diameter. The main reason, as shown in Fig. 10, is that in the IEM, the area bounded by the p - V diagram is smaller than that of the AEM. This bounded area represents the work done on the surroundings. Therefore, the AOP of the IEM is lower than that of the AEM. When the nozzle diameter is 0.15 mm, the minimum AOP is 0.4558 kW, which is 5.24 % lower than the AEM power of 0.4797 kW. With nozzle diameters of 0.25 mm and 0.35 mm, the AOPs are 0.4608 kW and 0.4704 kW respectively, representing decreases of 4.1 % and 1.98 % compared to AEM.
Fig. 11 Comparison of the effect of nozzle diameter on output performance
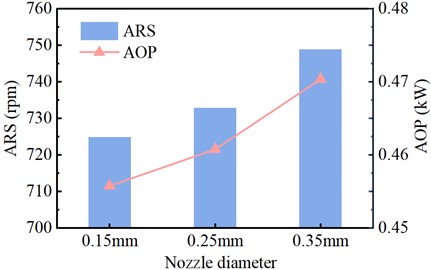
5.5. Effect of spray temperature on the SCTS-PE
The variation in spray temperature leads to different amounts of heat transferred by the injected water mist into the cylinder during a cycle, directly affecting the heat transfer rate between the gas and liquid. The following will elaborate in detail on the influence of spray temperature on the cylinder pressure, ARS, and AOP of the SCTS-PE.
5.6. Effect of spray temperature on the cylinder pressure of the SCTS-PE
The cylinder pressure of IEM is different under different spray temperatures. Fig. 12 shows the p-V diagram illustrating the impact of nozzle diameter on the cylinder pressure.
Fig. 12 Comparison of p-V diagrams for different spray temperature
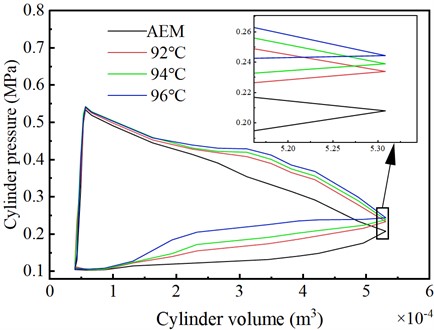
From Fig. 12, during the intake process, the cylinder air pressure of the different spray temperatures in the IEM is generally similar and slightly higher than that of the AEM. This indicates that different spray temperatures have a minor impact on the gas in the intake phase. During the expansion process, the cylinder air pressure of the different spray temperatures in the IEM is higher than that of the AEM. The higher the temperature of the injected water mist, the slightly higher the cylinder air pressure during the expansion phase of the IEM. The exhaust pressure for AEM is 0.208 MPa. For the IEM, when the spray temperature is 92 ℃, 94 ℃, and 96 ℃, the exhaust pressures are 0.235 MPa, 0.239 MPa, and 0.244 MPa, respectively. These values indicate an increase of 12.98 %, 14.9 %, and 17.31 % compared to the AEM. During the exhaust phase, the higher the spray temperature, the higher the cylinder gas pressure in the IEM. This leads to stronger resistance from the gas to the piston’s work during the exhaust phase. These findings indicate that higher spray temperatures of the injected water mist effectively enhance the heat transfer rate from the liquid to the gas.
5.7. Effect of spray temperature on the ARS and AOP of the SCTS-PE
When studying the influence of spray temperature on the ARS and AOP of the expander, the data used are from the stable operation of the SCTS-PE. When the spray temperature is too low, the heat provided may not be sufficient to meet the energy required for internal tax exchange in the cylinder, resulting in suboptimal heat exchange efficiency. On the other hand, when the temperature is too high, the remaining heat may interfere with the expansion phase, impeding the piston’s positive work. Therefore, the spray temperatures adopted in this experiment are 92 °C, 92 °C, and 92 °C, respectively. Fig. 13 shows the comparison of the effects of AEM on the ARS and AOP of the SCTS-PE under different spray temperatures.
Fig. 13 Comparison of the effect of spray temperature on output performance
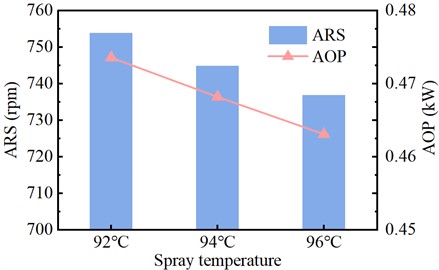
From Fig. 13, it can be observed that the ARS of the IEM is lower than that of the AEM. The ARS of the AEM is 764 rpm, while the ARS of the IEM are 754 rpm, 745 rpm, and 737 rpm respectively. The ARS of the IEM decreases as the spray temperature increases. This is mainly because a higher spray temperature can effectively improve the heat transfer rate of the liquid water. As a result, the pressure inside the SCTS-PE cylinder increases. However, due to the significant influence of cylinder pressure on the exhaust phase, the gas resistance to piston work during the exhaust process increases. Therefore, when the spray temperature is 96 °C, the ARS is relatively lower.
Under a constant load condition, the larger the ARS of the SCTS-PE, the greater the AOP of the SCTS-PE according to the power calculation formula. Fig. 13 illustrates the influence of different spray temperatures on the AOP of the SCTS-PE. From the figure, it can be seen that the AOP of the IEM at different spray temperatures is lower than that of the AEM. The AOP of the IEM decreases as the spray temperature increases. The main reason, as shown in Fig. 12, is that in the IEM, the area bounded by the p - V diagram is smaller than that of the AEM. This enclosed area represents the work done on the surroundings. Therefore, the AOP of the IEM is lower than that of the AEM. When the spray temperature is 96 °C, the minimum AOP is 0.4631 kW, which is 3.58 % lower than the AEM of 0.4797 kW. At spray temperatures of 92 °C and 94 °C, the AOPs achieved are 0.4736 kW and 0.4682 kW respectively, representing decreases of 1.29 % and 2.45 % compared to AEM.
5.8. Effect of spray timing on the SCTS-PE
The spray timing refers to the duration of injecting water mist during one cycle of system operation. The duration of injecting water mist can be controlled by the crankshaft angle formed by the rotation of the crankshaft. Starting and stopping the water mist at different crankshaft angles will have different effects on the system. Selecting the appropriate spray timing can enhance the output power of air expansion. The following will elaborate in detail on the influence of spray timing on the cylinder pressure, ARS, and AOP of the SCTS-PE.
5.9. Effect of spray timing on the cylinder pressure of the SCTS-PE
The different spray timing has a greater impact on the cylinder pressure. Fig. 14 shows the p - V diagram illustrating the impact of the cylinder pressure.
Fig. 14 Comparison of p-V diagrams for different spray timing
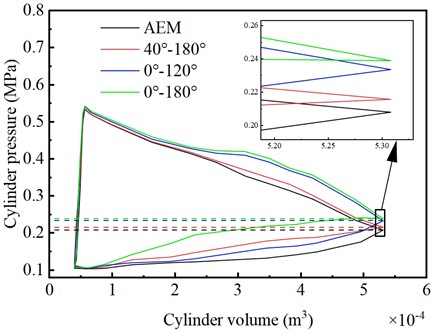
From Fig. 14, it can be observed that the exhaust pressure for the AEM is 0.208 MPa. However, for the IEMs with spray timings of 0°-180°, 0°-120°, and 40°-180°, the exhaust pressures are 0.239 MPa, 0.233 MPa, and 0.216 MPa, respectively. Compared to AEM, these values increased by 14.9 %, 12.02 %, and 3.85 %, respectively. Before the exhaust stage begins, the cylinder pressure of the IEM with a spray timing of 40°-180° is similar to that of the AEM. This is because the IEM injects less water mist during the intake stage with a spray timing of 40°-180°, resulting in insufficient heat exchange between the water mist and the air. On the other hand, compared to the AEM, the IEMs with spray timings of 0°-180° and 0°-120° have higher cylinder pressures during the intake stage, exceeding those of the IEM with a spray timing of 40°-180°. This is mainly because the water mist exchanges heat with the cylinder air throughout the entire intake stage. These results indicate that injecting a fine mist at the beginning of the intake process is more favorable for gas expansion, which also leads to higher cylinder pressure during the exhaust stage in the IEM compared to the AEM. This is because the injected water mist in the IEM participates in heat exchange with the cylinder air during the exhaust stage.
5.10. Effect of spray timing on the ARS and AOP of the SCTS-PE
When studying the influence of spray timing on the ARS and AOP of the SCTS-PE, the data used are from the stable operation of the SCTS-PE. Fig. 15 shows the comparison of the effects of AEM on the ARS and AOP of the SCTS-PE under different spray timing.
From Fig. 15, it can be seen that when the spray timing is 0°-120°, the ARS of the IEM is higher than that of the AEM. When the spray timing is 0°-180° and 40°-180°, the ARS of the IEM is lower than that of the AEM. The main reason is that under the 0°-120° spray timing, less water mist is injected during the intake and expansion phases, which promotes efficient heat exchange between the water mist and air. Only a small amount of residual water mist enters the exhaust phase, resulting in minimal impact on the exhaust phase and less negative work done by the gas on the piston. In contrast, in the other two spray timings, a large amount of residual water mist enters the exhaust phase and undergoes heat exchange with the gas, resulting in higher pressure inside the cylinder and more negative work done. Therefore, the ARS is lower in the IEM compared to the AEM.
Fig. 15 Comparison of the effect of spray timing on output performance
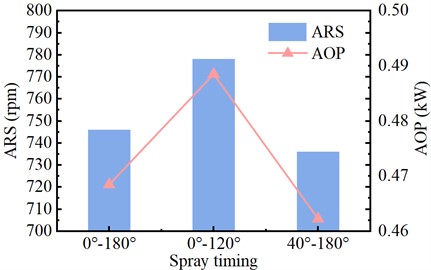
Under a constant load condition, the larger the ARS of the expander, according to the power calculation formula, the greater the AOP of the SCTS-PE. Fig. 15 illustrates the influence of different spray timings on the AOP of the SCTS-PE. When the spray timing is 0°-120°, the AOP of the IEM is 0.4885 kW, which is a 1.84% increase compared to AEM. When the spray timing is 0°-180° and 40°-180°, the AOP of the IEM is 0.4685 kW and 0.4623 kW, representing decreases of 2.39 % and 3.76 % respectively compared to AEM. The main reason for these results, as seen in Fig. 14, is that in the IEM, the area enclosed by the p-V diagram for the 0°-120° spray timing is larger than that of the AEM. The enclosed area represents the work done on the surroundings. Therefore, under this spray timing, the AOP of the IEM is greater than that of the AEM. On the other hand, the area enclosed by the p-V diagram for the 0°-180° and 40°-180° spray timings is smaller than that of the AEM. Hence, the AOP of the IEM is lower than that of the AEM for these two spray times.
6. Conclusions
This paper presents an experimental study on SCTS-PE based on in-cylinder spray heat transfer. Firstly, the influence of different load torques on the SCTS-PE output power is investigated. Then, a single-variable analysis is conducted on three parameters of the spray system: nozzle diameter, spray temperature, and spray timing. The study examines the effects of these individual parameters on cylinder pressure, ARS, and AOP. The following conclusions are drawn from the experimental analysis:
1) Under the influence of different loads, both the AOP of the IEM and the AEM increase with increasing load. Moreover, the AOP of the IEM is lower than that of the AEM, with reductions of 2.22 %, 3.30 %, 2.08 %, 2.32 %, and 2.84 % as the load increases.
2) Under the influence of different nozzle diameters, the exhaust pressure of the IEM is higher than that of the AEM, with increases of 14.9 %, 13.46 %, and 11.54 % respectively. However, the cylinder pressure during the exhaust phase remains higher in the IEM, with a greater impact compared to the intake and expansion phases. Consequently, the ARS and AOP of the IEM are lower than those of the AEM. The AOP decreases by 5.24 %, 4.10 %, and 1.98 % respectively for different nozzle diameters, while the AOP of the IEM increases with larger nozzle diameters.
3) Under the influence of different spray temperatures, the exhaust pressure of the IEM is higher than that of the AEM, with increases of 12.98 %, 14.9 %, and 17.31 % respectively. The ARS and AOP of the IEM are lower than those of the AEM. The AOP decreases by 1.29 %, 2.45 %, and 3.58 % respectively for different spray temperatures, while the AOP of the IEM decreases with increasing spray temperature.
4) Under the influence of different spray timings, the exhaust pressure of the IEM is higher than that of the AEM, with increases of 14.9 %, 12.02 %, and 3.85 % respectively. However, during the exhaust phase, the cylinder pressure is significantly higher for a spray timing of 40°-180° compared to the other two timings. When the spray timing is 0°-120°, the AOP of the IEM is higher than that of the AEM, with an increase of 1.84 %. When the spray timing is 0°-180° and 40°-180°, the AOP of the IEM is lower than that of the AEM. The minimum AOP is 0.4623 kW for a spray timing of 40°-180°, representing a reduction of 3.76 % compared to AEM.
5) The IEM can increase the pressure in the cylinder, but it has a greater impact on the exhaust stage. Excessive exhaust pressure reduces the AOP of the SCTS-PE, but the AOP of the IEM with appropriate spray timing can be greater than that of the AEM. The ideal spraying timing is 0°-120°, and the AOP of IEM has increased by 1.84 %.
- Y. Shi, “China’s annual wind and photovoltaic power generation has reached a historic high,” (in Chinese), Petroleum and New Energy , Vol. 35, No. 1, pp. 12–16, 2023. Search CrossRef
- Z. Tong, Z. Cheng, and S. Tong, “A review on the development of compressed air energy storage in China: Technical and economic challenges to commercialization,” Renewable and Sustainable Energy Reviews , Vol. 135, p. 110178, Jan. 2021, https://doi.org/10.1016/j.rser.2020.110178 Publisher
- S. W. Mei et al., “Research and engineering practice of non-supplementary combustion compressed air energy storage: Taking Jintan national demonstration project as an example,” (in Chinese), Experimental Technology and Management , Vol. 39, No. 5, pp. 1–8, 2022. Search CrossRef
- B. Huang, X. Qiu, W. Wang, H. Li, and W. Zhou, “Overview of research situation and progress on compressed air energy storage technology,” in IOP Conference Series: Earth and Environmental Science , Vol. 295, No. 2, p. 012020, Jul. 2019, https://doi.org/10.1088/1755-1315/295/2/012020 Publisher
- M. Budt, D. Wolf, R. Span, and J. Yan, “A review on compressed air energy storage: Basic principles, past milestones and recent developments,” Applied Energy , Vol. 170, pp. 250–268, May 2016, https://doi.org/10.1016/j.apenergy.2016.02.108 Publisher
- M. Heidari, M. Mortazavi, and A. Rufer, “Design, modeling and experimental validation of a novel finned reciprocating compressor for Isothermal Compressed Air Energy Storage applications,” Energy , Vol. 140, pp. 1252–1266, Dec. 2017, https://doi.org/10.1016/j.energy.2017.09.031 Publisher
- C. Qin and E. Loth, “Simulation of spray direct injection for compressed air energy storage,” Applied Thermal Engineering , Vol. 95, pp. 24–34, Feb. 2016, https://doi.org/10.1016/j.applthermaleng.2015.11.008 Publisher
- Q. He and K. Wang, “Research progress of isothermal compressed air energy storage technology,” Thermal Power Generation , Vol. 51, No. 8, pp. 11–19, 2022. Search CrossRef
- O. N. Igobo and P. A. Davies, “Review of low-temperature vapour power cycle engines with quasi-isothermal expansion,” Energy , Vol. 70, pp. 22–34, Jun. 2014, https://doi.org/10.1016/j.energy.2014.03.123 Publisher
- E. M. Gouda, Y. Fan, M. Benaouicha, T. Neu, and L. Luo, “Review on liquid piston technology for compressed air energy storage,” Journal of Energy Storage , Vol. 43, p. 103111, Nov. 2021, https://doi.org/10.1016/j.est.2021.103111 Publisher
- W. He and J. Wang, “Optimal selection of air expansion machine in compressed air energy storage: a review,” Renewable and Sustainable Energy Reviews , Vol. 87, pp. 77–95, May 2018, https://doi.org/10.1016/j.rser.2018.01.013 Publisher
- X. Zhang, Y. Xu, J. Xu, H. Xue, and H. Chen, “Study of a single-valve reciprocating expander,” Journal of the Energy Institute , Vol. 89, No. 3, pp. 400–413, Aug. 2016, https://doi.org/10.1016/j.joei.2015.02.013 Publisher
- A. T. Rice, P. Y. Li, and C. J. Sanckens, “Optimal efficiency-power tradeoff for an air compressor/expander,” Journal of Dynamic Systems, Measurement, and Control , Vol. 140, No. 2, p. 02101, Feb. 2018, https://doi.org/10.1115/1.4037652 Publisher
- J. Wieberdink, P. Y. Li, T. W. Simon, and J. D. van de Ven, “Effects of porous media insert on the efficiency and power density of a high pressure (210 bar) liquid piston air compressor/expander – an experimental study,” Applied Energy , Vol. 212, pp. 1025–1037, Feb. 2018, https://doi.org/10.1016/j.apenergy.2017.12.093 Publisher
- H. Chen, Y.-H. Peng, Y.-L. Wang, and J. Zhang, “Thermodynamic analysis of an open type isothermal compressed air energy storage system based on hydraulic pump/turbine and spray cooling,” Energy Conversion and Management , Vol. 204, p. 112293, Jan. 2020, https://doi.org/10.1016/j.enconman.2019.112293 Publisher
- P. Zhao, Y. Lai, W. Xu, S. Zhang, P. Wang, and J. Wang, “Performance investigation of a novel near‐isothermal compressed air energy storage system with stable power output,” International Journal of Energy Research , Vol. 44, No. 14, pp. 11135–11151, Aug. 2020, https://doi.org/10.1002/er.5633 Publisher
- B. Bollinger, “Demonstration of isothermal compressed air energy storage to support renewable energy production,” Office of Scientific and Technical Information (OSTI), Technology performance report, Jan. 2015. Publisher
- X. Zhang et al., “A near-isothermal expander for isothermal compressed air energy storage system,” Applied Energy , Vol. 225, pp. 955–964, Sep. 2018, https://doi.org/10.1016/j.apenergy.2018.04.055 Publisher
- C. Braasch, W. Nieratschker, M. Nadler, and D. Nett, “Experimental and numerical investigation of heat transfer by water spray injection into pressurized gas atmospheres,” Applied Thermal Engineering , Vol. 214, p. 118682, Sep. 2022, https://doi.org/10.1016/j.applthermaleng.2022.118682 Publisher
- Q. Yu, X. Li, Y. Geng, and X. Tan, “Study on quasi-isothermal expansion process of compressed air based on spray heat transfer,” Energy Reports , Vol. 8, pp. 1995–2007, Nov. 2022, https://doi.org/10.1016/j.egyr.2022.01.019 Publisher
- Q. Yu, M. Cai, Y. Shi, and Q. Xu, “Optimization study on a single-cylinder compressed air engine,” Chinese Journal of Mechanical Engineering , Vol. 28, No. 6, pp. 1285–1292, Jul. 2015, https://doi.org/10.3901/cjme.2015.0520.072 Publisher
- Q. Yu, M. Cai, Y. Shi, and Z. Fan, “Optimization of the energy efficiency of a piston compressed air engine,” Strojniški vestnik – Journal of Mechanical Engineering , Vol. 60, No. 6, pp. 395–406, Jun. 2014, https://doi.org/10.5545/sv-jme.2013.1383 Publisher
- Z. F. Huang, W. Tan, S. J. Jiang, Y. H. Ding, S. Zheng, and Q. Y. Hou, “Vortexer flow test uncertainty evaluation and optimal formula validation,” Measurement & Control Technology , Vol. 43, No. 7, pp. 55–64, 2024. Search CrossRef
About this article
The research work presented in this paper is financially supported by a Grant (52065054) from the National Natural Science Foundation of China and a Grant (2022LHMS05023) from the Natural Science Foundation of Inner Mongolia.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Qihui Yu: conceptualization, formal analysis, funding acquisition, resources, writing-review and editing. Jiabao Zhang: writing-original draft preparation, investigation, supervision. Xiaodong Li: methodology, validation. Guoxin Sun: visualization. Ripeng Qin: software. Feng Li: project administration.
The authors declare that they have no conflict of interest.
Related Articles
- Skip to main content
- Keyboard shortcuts for audio player
2024 Election
The debate between harris and trump wasn’t close — and 4 other takeaways.

Domenico Montanaro

Former President Donald Trump, the Republican presidential nominee, and Vice President Kamala Harris, the Democratic nominee, participate during ABC News' presidential debate Tuesday at the National Constitution Center in Philadelphia. Alex Brandon/AP hide caption
Well, that was different from the June 27 debate between President Biden and Donald Trump.
If that June debate was a five-alarm fire for Democrats that eventually forced Biden from the race, after Tuesday’s debate between Trump and Vice President Kamala Harris, Trump’s proponents should probably check the temperature in their own house.
What happened — and what could it mean going forward?
Here are 5 takeaways:
1. This debate wasn’t close.
The majority of the focus coming into Tuesday was about how Harris would handle her first-ever presidential debate with someone who had been on this stage many times. Could she answer questions about her position shifts; parry attacks from Trump, someone who tries to be the alpha on these stages; could she answer the attack that she’s light on policy; and could she appear “presidential”?

NPR fact-checked the Harris-Trump presidential debate. Here's what we found
She may have seemed nervous at first, but she quickly found her voice and more than acquitted herself well. All of those questions were quickly dispatched:
- She explained her shift on fracking (“My position is that we have got to invest in diverse sources of energy, so we reduce our reliance on foreign oil”).
- Harris was far more dominant than Trump, from beginning to end. She called him “weak and wrong,” inverting the political cliché that “strong and wrong” beats “weak and right.” Harris answered questions, then redirected and baited him on a host of issues.
- She got under Trump’s skin — something he usually tries to do — by saying that people at his rallies leave “early out of exhaustion and boredom,” painting him as out of touch and a bad businessman for inheriting $400 million “on a silver platter and then filed for bankruptcy six times,” and chiding him for being “fired by 81 million people” in the 2020 election and now being “confused” about losing.
- Harris addressed policy, including tax breaks for small businesses and parents and touting her idea for a first-time home-buyer credit for down payments. She repeatedly said, “I have a plan,” while Trump was left saying, “I have concepts of a plan” when it comes to replacing the Affordable Care Act.
- And on the presidential question — Harris was calm, in command and in control and looked to the future, distinguishing herself from both Biden and Trump.
Trump’s team ahead of the debate equated the Republican standard-bearer to boxing great Muhammad Ali. If he was a boxer, Trump was cut and bleeding in the middle of the fight, and by the end, was TKO’d. Or as a Democratic strategist texted afterward, it was more like Ali vs. Berbick , Ali’s last fight, decided unanimously — for Berbick.
Trump made the unusual move for a presidential candidate to go into the spin room after the debate and talk to reporters. That’s not something that’s normally done when someone has a good debate. That’s usually reserved for low-polling primary candidates, who felt they didn’t get enough time or attention during the debate.
2. The spotlight should now be on Trump’s incoherence and general lack of any serious grasp on policy.
Coming into the debate, we noted that if Harris is “able to acquit herself passably, the spotlight and scrutiny should be heavily on Trump.”
That’s because Trump did not have a very good debate against Biden in June, but his serious problems — his lack of substance and repeated lies — were overshadowed by Biden’s disastrous performance, maybe the worst of any presidential candidate in history.

Taylor Swift endorses Kamala Harris in Instagram post after the debate
With a more-than-competent performance from Harris Tuesday, Trump’s lies, meandering, conspiracies and often general incoherence was made even more glaring.
He wandered through conspiracies about, not just the election, but also about who is currently president (Joe Biden), the usual about immigrants who (aren’t actually) coming from “mental institutions and insane asylums” and the newly unusual ( and debunked ) about immigrants who (are not) “eating the dogs” or “cats.”
Trump got the conspiracy wrong , though, because it was about ducks, not dogs.
Trump even got wrong the actual facts of Harris’ misleading charge that Trump predicted “a bloodbath” if the outcome of this election is “not to his liking.”
“It was a different term,” Trump said, “and it was a term that related to energy because they have destroyed our energy business.”
It was the correct term. He did say “bloodbath” back in March , but he was talking in the context of Chinese tariffs, the auto industry and a transition to electric vehicles — not “our energy business.”
It’s the very kind of thing that would have had Democrats nervous about their octogenarian former candidate and Republicans “outraged” on cable news about Biden’s mental state.
3. Trump was on the defensive and evasive, even on issues that should benefit him — and didn’t land much, if anything, that stuck.
Harris had Trump on the defensive from the get-go on the economy (about his tax cuts and tariffs), his jobs record, his handling of the pandemic and Jan. 6. There were times, even on immigration, when Trump decided to address a Harris attack instead of talking about the issue he ostensibly wants to talk most about.
For someone who likes to bill himself a straight shooter, Trump didn’t answer questions directly and dumped a greatest hits of lies from this campaign. He declined to say if he wanted Ukraine to win against Russia, wouldn’t answer if he had any regrets about his response to the violence on Jan. 6, and he twice refused to say if he would veto a national abortion ban, like his vice-presidential running mate said he would.

Trump repeats the false claim that Democrats support abortion 'after birth' in debate
In fact, he went out of his way to say essentially that Republican vice-presidential candidate JD Vance doesn’t speak for him — in a clumsy and meandering way that led him to student loans:
“Well, I didn't discuss it with JD in all fairness. JD — And I, I don't mind if he has a certain view, but I think he was speaking for me, but I really didn't. Look, we don't have to discuss it, because she'd never be able to get it, just like she couldn't get student loans. They couldn't get student loans. They didn't even come close to getting student loans. They taunted young people and a lot of other people that had loans. They can never get this approved. So it doesn't matter what she says about going to Congress. So wonderful, let's go to Congress, do it.”
Never mind that Republicans in Congress would not act to help relieve student loans or that Republican-led states sued to end Biden’s executive action on student-loan forgiveness. But Trump was digging the hole even deeper for himself on abortion rights.
“I did a great service in doing it,” Trump said about the overturning of Roe . “It took courage to do it. And the Supreme Court had great courage in doing it. And I give tremendous credit to those six justices.”
Nearly two-thirds have said they opposed the overturning of Roe .
Trump was also outside the mainstream of public opinion in talking about the Affordable Care Act. He called it “lousy” and “not very good today” when record numbers of people have a favorable opinion of it.
Trump’s best attack was probably this:
“She's gonna do all these wonderful things,” he said. “Why hasn't she done it? She's been there for three-and-a-half years. They've had three-and-a-half years to fix the border. They've had three-and-a-half years to create jobs and all the things we talked about. Why hasn't she done it?”
But a coherent attack line was rare from Trump Tuesday night. And even this one was nearly a concession.

Facial expressions spoke volumes when mics were muted in the presidential debate
4. the moderators fact-checked unlike in the previous debate..
CNN said it was going to leave the fact checking to the candidates during the June debate between Trump and Biden.
ABC took a different approach. Moderators David Muir and Linsey Davis interjected with fact checks four times — all were of Trump.
That was not a reflection of bias; it was because of just how many things Trump said there were blatantly false, like on crime statistics, the dogs and cats conspiracy and the 2020 election.
They did it with a mild, but clear tone and maintained control of the debate throughout the evening, getting to lots of topics and not letting either candidate run over them.
Their approach was notable, particularly with viewership expected to be high. When he went to the spin room, Trump added to his pile of grievances, claiming the debate was “very unfair” and called it “three on one.”
5. Harris has done everything right — and could still lose.
Harris arguably handled Trump better than anyone has at a debate, whether it was Hillary Clinton in 2016 or Biden in 2020 — even though most concluded that Clinton and Biden won most, if not all, of those face-offs.
Since getting into this shortened campaign, Harris has done pretty much everything right. She’s tacked to the middle, raised more than half-a-billion dollars, staffed up and opened field offices across the swing states, fired up the Democratic base and now even out-debated Trump.
But the political reality is Harris could still lose.

NPR poll shows why the stakes are so high for Harris and Trump in the debate
Trump has a strong and devoted base, and the seven swing states — Pennsylvania, Michigan, Wisconsin, North Carolina, Georgia, Arizona and Nevada — are more conservative than the country at large.
People still are more pessimistic than optimistic on the economy, even if that’s improved some lately, and polls — including the NPR/PBS NewsHour/Marist poll out Tuesday — have shown people trust Trump to handle the economy, immigration and the war in the Middle East more than Harris.
Could this debate have changed some minds? Maybe. But views of Trump have been ingrained. This race is very much a coin flip, according to the polls, and that’s unlikely to change very much even after this debate, because of how hyper-polarized this country is.
Correction Sept. 11, 2024
An earlier version of this story misspelled ABC moderator Linsey Davis' name.
- election 2024

COMMENTS
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater ...
An example of results from a single-case A 1 B 1 A 2 B 2 study conducted on two participants with severe unilateral neglect after a right-hemisphere stroke. Two weeks of conventional treatment (baseline phases A 1, A 2 ) alternated with two weeks of visuo-spatio-motor cueing (intervention phases B 1 , B 2 ).
Presentation of Case. Dr. Scott B. Silverman: A 68-year-old man was admitted to this hospital because of worsening confusion. The patient had a history of hypertension and coronary artery disease ...
CASE 1. A 20 year old man with no past medical history presented to a primary stroke center with sudden left sided weakness and imbalance followed by decreased level of consciousness. Head CT showed no hemorrhage, no acute ischemic changes, and a hyper-dense basilar artery. CT angiography showed a mid-basilar occlusion.
A patient with a complete motor deficit of the right upper limb after stroke was followed for 12 years. He presented a remarkable late recovery of the upper-limb motility, in terms of strength, individual finger movement, and manual dexterity, 5 years after stroke onset. The aim of the present study was to assess objectively the upper-limb ...
Training-induced neural dynamics was also tracked in a single-case study of a ... on improve balance among chronic stroke patients. This study is done by one-test method on the 6 patients with a ...
To our knowledge, the adoption of Learning Health System (LHS) concepts or approaches for improving stroke care, patient outcomes, and value have not previously been summarized. This topical review provides a summary of the published evidence about LHSs applied to stroke, and case examples applied to different aspects of stroke care from high and low-to-middle income countries. Our attempt to ...
Purpose.: This study explored whether the LSVT BIG program could lead to improved performance in client-identified occupations and decreased impairment late poststroke. Method.: A single-case experimental design with one repetition was completed. Participants were two adults who had experienced a stroke 3 and 12 years previously.
Abstract. A 55-year-old male subject was treated with a two-tiered neurotherapy approach for a period of six months beginning approximately one year after a left-side CVA. Medical evaluation revealed left posterior temporal/parietal infarctions secondary to occlusion of the left internal carotid artery. The patient complained of hesitant speech ...
Presents the case of a 55-yr-old male treated with a 2-tiered neurotherapy approach for 6 mo beginning approximately 1 yr after a left-side cerebrovascular accident. The patient complained of hesitant speech with word finding difficulty and paraphasia, difficulty focusing his right eye, lack of balance and coordination, poor short-term memory, poor concentration, anxiety, depression, and ...
Single-case experimental designs (SCED) are experimental designs aiming at testing the effect of an intervention using a small number of patients (typically one to three), using repeated measurements, sequential (± randomized) introduction of an intervention and method-specific data analysis, including visual analysis and specific statistics.The aim of this paper is to familiarise ...
Safety of repeated sessions of galvanic vestibular stimulation following stroke: a single-case study Brain Inj. 2009 Sep;23(10):841-5. doi: 10.1080/02699050903232541. ... The aim of the present study was to assess whether this increased exposure is well-tolerated and consistent with patient well-being.
Biofeedback and Self-Regulation, Vol. 20, No. 3, 1995 Neurotherapy for Stroke Rehabilitation: A Single Case Study a George R. Rozelle 2 and Thomas H. Budzynski 3 Anabasis, Sarasota, Florida, and Center for Behavioral Medicine, University of West Florida, Pensacola, Florida A 55-year-old male subject was treated with a two-tiered neurotherapy approach for a period of six months beginning ...
Abstract. A 37-year-old female with a history of complex trauma, anxiety and depression was treated with Emotional Freedom Techniques (EFT) supplemented with guided imagery within the first 24 hours of having a stroke that affected the right side. CT scans indicated a hemorrhage and brain clot. Surgery was delayed as another seizure was expected.
Received: June 17, 2021. Accepted: October 13, 2021. Published: October 26, 2021. Abstract. A 37-year-old female with a history of complex trauma, anxiety and depression was treated. with ...
We compared 961 patients with a first‐ever IS at 25 to 49 years to 1403 frequency‐matched stroke‐free controls from a population‐based cohort study (FINRISK).Assessed risk factors included an active malignancy, atrial fibrillation, cardiovascular disease, current smoking status, a family history of stroke, high low‐density lipoprotein cholesterol, high triglycerides, low high ...
Read chapter 7 of Patient Management in the Telemetry/Cardiac Step-Down Unit: A Case-Based Approach online now, exclusively on AccessMedicine. AccessMedicine is a subscription-based resource from McGraw Hill that features trusted medical content from the best minds in medicine.
Finally, it is important to acknowledge that this study employed a single-case design with a limited sample size of 10 participants, signifying the need for larger-scale research (i.e., a Phase II randomized controlled trial) to further validate these findings and enhance their generalisability.
In Uganda, literature on stroke in young adults is limited however results of a study done among acute stroke patients admitted to the national referral hospital (Mulago hospital) showed a 30-day mortality of 43.8%. Out of 133 patients, 32 patients (25%) were less than 51 years old. Out of the 56 patients that died, 13 patients (23%) were less ...
Other hypothesised reasons for stroke development in COVID-19 patients are the development of hypercoagulability, as a result of critical illness or new onset of arrhythmias, caused by severe infection. Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer.
In this single-centre retrospective cohort study, there was no difference in functional outcomes at 6 months post-stroke between the group that had a DC within 48 h of acute ischaemic stroke onset and the group that had a DC more than 48 h after an acute ischaemic stroke. In a study of malignant middle cerebral artery infarction, Elsawaf et al ...
A 55-year-old male subject was treated with a two-tiered neurotherapy approach for a period of six months beginning approximately one year after a left-side CVA. Medical evaluation revealed left posterior temporal/parietal infarctions secondary to occlusion of the left internal carotid artery. The patient complained of hesitant speech with word finding difficulty and paraphasia, difficulty ...
Introduction Stroke is a potentially debilitating complication of heart valve replacement surgery, with rates ranging from 1 to 10%. Despite advancements in surgical techniques, the incidence of postoperative stroke remains a significant concern, impacting patient outcomes and healthcare resources. This study aims to investigate the incidence, risk factors, and outcomes of in-hospital adverse ...
Objectives Guidelines in several countries recommend against driving soon after a stroke; however, some patients resume driving within one month after onset. This study aimed to examine the relationship between neurological and social background factors at intensive care unit (ICU) admission and resumption of motor vehicle driving within 30 days of the first acute stroke/cerebral hemorrhage ...
This study aimed to address this concern and to evaluate whether an intervention of maximal intensity cycling exercise impaired an individual's ability to actively extend his hemiparetic elbow. Using a single case design, it was shown that active elbow extension improved during the period of this investigation, and was not impaired immediately ...
A single-case A-B study design was used, repeated across the four participants. Expressive use of the target words was probed during the baseline (A) and intervention (B) phases. Following Girolametto et al. ( Citation 1996 ), a control behaviour (expressive use of untrained control words) was also probed throughout the baseline and ...
Objectives and Outline of Case Study. Yin points out the value of the case study as a research method, particularly "when the focus is on a contemporary phenomenon within some real-life context" (p. 1). This study utilized Yin's single case study approach to consider the deliberate development and influence of a values-based culture and ...
The cylinder diameter of the single-cylinder two-stroke PE is 0.085 m, the cylinder stroke is 0.088m, and the cylinder clearance is 3.97×10-5 m. The cylinder head of the expander is equipped with a nozzle head and a miniature dynamic pressure transmitter, and the cylinder head is shown in Fig. 7.
The debate between Harris and Trump wasn't close — and other takeaways Tuesday's debate between the current vice president and former president was a clear contrast from the June debate that ...